Waking up with stiff, swollen fingers or wrists that loosen only after an hour or two is more than an annoyance; it can be the earliest signal of rheumatoid arthritis (RA). RA is an autoimmune disease that affects the lining of the joints, causing pain, swelling, and eventually damage if left untreated. Early recognition and prompt care are crucial to slowing disease progression and preserving quality of life.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis is a chronic inflammatory disorder in which the immune system mistakenly attacks the synovium, the lining of the membranes that surround joints. Unlike osteoarthritis, which is mainly caused by wear-and-tear, RA is systemic and can affect other organs over time. Symptoms often appear symmetrically (both hands, both knees) and typically include prolonged morning stiffness, joint swelling, and fatigue.
RA affects roughly 0.5–1% of the adult population worldwide and can begin at any age, though onset is most common between ages 30 and 60. Women are affected more often than men, and prognosis has improved substantially over the past two decades, thanks to earlier diagnosis and more effective medications.
 Recognizing the Early Symptoms
Recognizing the Early Symptoms
Morning Stiffness and Prolonged Stiffness
Morning stiffness that lasts 30 minutes or longer, often for several hours, is a hallmark of inflammatory arthritis like RA. The stiffness tends to improve with movement and activity as the day goes on, which contrasts with degenerative arthritis, where stiffness may be short-lived or triggered by inactivity only.
Symmetric Joint Swelling and Pain
RA commonly affects small joints first: the wrists, the proximal interphalangeal (middle) joints and metacarpophalangeal (base) joints of the hands, and the feet. Symptoms are often symmetric, meaning the same joints on both sides of the body are affected. Swelling can be soft and boggy due to inflamed synovium, and joints may feel warm to the touch.
Systemic Signs: Fatigue, Low-Grade Fever, Loss of Function
Because RA is systemic, it frequently causes general symptoms such as persistent fatigue, a low-grade fever, and a sense of being unwell. Morning stiffness combined with reduced grip strength, difficulty opening jars, or trouble buttoning a shirt suggests the condition is impacting day-to-day function.
What Causes Rheumatoid Arthritis?
RA arises from a complex interaction between genetic susceptibility, environmental triggers, and immune system dysregulation. Specific genes (for example, variants in the HLA-DRB1 gene) are associated with a higher risk. Smoking is a well-established environmental risk factor that increases both the likelihood of developing RA and disease severity. Other potential triggers include infections and hormonal factors.
Autoantibodies are a key part of RA biology. Rheumatoid factor (RF) and anti–cyclic citrullinated peptide (anti-CCP, or ACPA) antibodies can be detected in many people years before clinical symptoms appear. Their presence can predict more aggressive disease and joint damage over time.
How Rheumatoid Arthritis Is Diagnosed
Clinical Evaluation
Diagnosis begins with a careful clinical history and physical examination. Physicians will ask about the pattern and timing of symptoms, family history of autoimmune diseases, and functional limitations. The examination focuses on joint swelling, tenderness, range of motion, and symmetry of involvement.
Laboratory Tests
Blood tests support the diagnosis and help characterize disease activity. Common tests include:
Rheumatoid factor (RF): positive in many but not all patients.
Anti-CCP (ACPA): more specific for RA and often associated with more severe disease.
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP): markers of systemic inflammation.
Complete blood count: to look for anemia of chronic disease or other abnormalities.
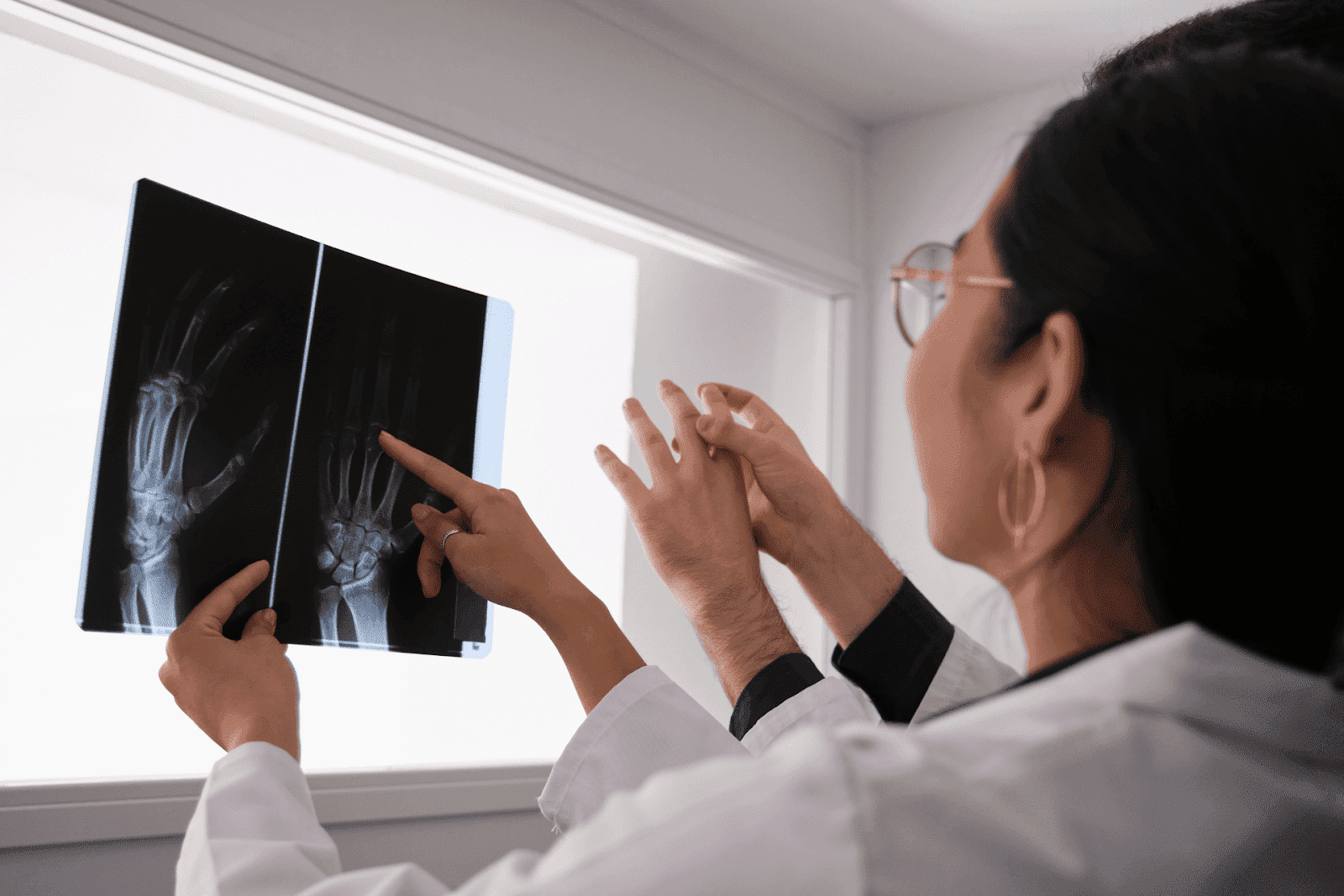
Imaging Studies
X-rays may show joint space narrowing and erosions in established disease, but early RA changes can be subtle. Ultrasound and magnetic resonance imaging (MRI) are more sensitive for detecting synovitis, tendon inflammation, and early erosions, and are increasingly used when clinical suspicion is high despite normal X-rays.
 Treatment Principles: Suppress Inflammation, Prevent Damage
Treatment Principles: Suppress Inflammation, Prevent Damage
The main goals of RA treatment are to reduce inflammation, relieve symptoms, prevent joint and organ damage, and preserve function and quality of life. Treatment is tailored to each person’s disease severity, comorbidities, and personal goals.
Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs are the cornerstone of RA care because they slow disease progression and reduce the risk of joint damage. Methotrexate is commonly used as first-line therapy, often combined with folic acid to reduce side effects. If methotrexate alone is insufficient, combinations of traditional DMARDs or the addition of biologic DMARDs (such as TNF inhibitors, IL-6 inhibitors, and others) or targeted synthetic DMARDs (like JAK inhibitors) are considered.
Short-Term Symptom Control
During flares, short-term use of corticosteroids can rapidly reduce inflammation and provide symptom relief. Nonsteroidal anti-inflammatory drugs (NSAIDs) and analgesics help manage pain but do not alter disease progression. Long-term steroid use is avoided when possible because of side effects.
Nonpharmacologic Approaches
Physical therapy, occupational therapy, and lifestyle modifications are essential complements to medication. Exercise programs that emphasize low-impact aerobic activity, strength training, and joint protection help maintain mobility. Occupational therapists can suggest assistive devices, adaptive techniques, and splints to protect joints and preserve function.
Living Well with RA: Practical Strategies
RA is a chronic condition, but many people achieve excellent control with modern therapy. A combination of medication, lifestyle changes, and regular monitoring provides the best chance to stay active and limit disability.
Exercise and Joint Care
Regular movement keeps joints flexible and muscles strong. Low-impact activities like walking, swimming, and cycling are joint-friendly. Strength training builds supportive musculature while range-of-motion exercises prevent stiffness. Balance exercises reduce fall risk, which matters because weakened joints are more vulnerable to injury.
Nutrition and Risk Factor Management
A balanced diet rich in omega-3 fatty acids, fruits, vegetables, and whole grains supports overall health and may reduce inflammation. Smoking cessation is a top priority for people with RA because smoking worsens disease activity and reduces the effectiveness of some therapies. Managing comorbid conditions like hypertension, diabetes, and high cholesterol is also important.
Mental Health and Social Support
Chronic pain and disability can take an emotional toll. Access to counseling, support groups, or peer networks helps people cope with anxiety, depression, and the day-to-day challenges that accompany a chronic illness. Work accommodations and assistive technologies often make it possible to maintain employment and independence.
When to See a Clinician, Don’t Wait
Early referral to a rheumatologist is crucial when RA is suspected. Delaying treatment by months or years increases the risk of irreversible joint damage. Seek prompt evaluation if there is persistent morning stiffness lasting more than 30 minutes, symmetric joint swelling, unexplained fatigue combined with joint pain, or progressive loss of function.
For urgent symptoms such as high fever, sudden visual changes, severe shortness of breath, or signs of infection while on immunosuppressive therapy, immediate medical attention is required.
Quick Access to Evaluation and Guidance
Telehealth has expanded access to medical evaluation, and it can play an important role in the early recognition and management of RA. Virtual visits are convenient for initial symptom assessment, medication counseling, and routine follow-up when an in-person examination is not required.
Doctronic offers both free AI-driven consultations and low-cost telehealth video visits with licensed clinicians across all 50 states. The AI doctor can provide an immediate, evidence-based initial assessment and suggest next steps, such as lab tests or a referral to rheumatology, in seconds. For a more personal visit, Doctronic also provides inexpensive (<$40) video visits with doctors 24/7, enabling timely care without the need to travel.
When Telehealth Is Appropriate
Telehealth is well-suited for initial symptom triage, discussing laboratory results, medication adjustments, and monitoring disease control. It’s especially useful for people who live far from specialists, have mobility challenges, or need quick guidance outside of standard office hours.
Limitations of Telehealth
Remote visits cannot fully replace in-person joint examinations or imaging that may be required for diagnostic confirmation. Certain urgent issues require in-person care or immediate emergency services. Doctronic’s AI and telehealth services provide rapid assessment and help determine whether an in-person evaluation is necessary.
Visit Doctronic.ai to try the AI doctor for a fast initial assessment, or book an affordable video visit with a licensed clinician when a more personal encounter is needed. The AI service is free to use on the website, and over 10 million people have used the system so far, reflecting its rapid growth and broad acceptance.
Tests and Follow-Up: What to Expect After an Initial Telehealth Visit
Following a telehealth assessment that raises suspicion for RA, the next steps typically include blood tests (RF, anti-CCP, ESR, CRP, CBC) and imaging studies. These tests can often be arranged locally and reviewed during a follow-up telehealth or in-person appointment.
If laboratory or imaging results support RA, a referral to a rheumatologist is commonly recommended. Early initiation of DMARD therapy, often guided by a specialist, yields the best outcomes. Doctronic’s clinicians can assist in coordinating these next steps and help interpret test results, which streamlines the process of getting definitive care.
Medications and Safety Considerations
Many RA medications require monitoring because of potential side effects. For example, methotrexate necessitates periodic blood tests to monitor liver function and blood counts. Biologic therapies carry an increased infection risk and often require screening for latent tuberculosis and hepatitis before starting therapy.
Open communication with clinicians about infections, vaccinations, and planned surgeries ensures safety. Vaccination, when appropriate, helps prevent infections that can be more severe in people with RA, especially those on immunosuppressive medications.
When Disease Flares: Action Steps
Flares are periods of increased disease activity marked by worsening pain, swelling, and reduced function. During a flare, temporary adjustments to therapy (a short course of corticosteroids, medication timing changes) may be necessary. Telehealth is a fast way to obtain guidance during flares, but severe or rapidly worsening symptoms, such as inability to use a limb or signs of infection, should prompt urgent in-person evaluation.
Finding the Right Care Team
Optimal RA management is collaborative. A care team may include a rheumatologist, primary care clinician, physical and occupational therapists, pharmacists, and mental health professionals. Coordinated care helps address the whole person, not just joint inflammation, and improves long-term outcomes.
Early Action Matters
Morning stiffness and swollen joints are common complaints, but when symptoms are prolonged or progressive, they could indicate rheumatoid arthritis. Early recognition, timely testing, and prompt initiation of disease-modifying therapy reduce the risk of joint damage and disability.
Telehealth services and AI-driven assessments make it easier than ever to get an initial evaluation and a plan of action. For a fast, evidence-based assessment, try the AI doctor at Doctronic.ai or schedule an affordable telehealth video visit with a licensed clinician through Doctronic.ai. Quick engagement with medical care is the best way to protect joints and preserve a full, active life.
Get a Fast, Evidence-Based Check for Possible RA, Right Now
If morning stiffness or swollen joints have you worried, skip the wait and get an immediate, expert-backed assessment from Doctronic, the #1 AI Doctor. Our free AI visits synthesize the latest peer‑reviewed medicine to help you understand symptoms, suggest tests (RF, anti‑CCP, ESR/CRP) and next steps, and you can take the results to any clinician. When you need a personal touch, book an inexpensive (<$40) telehealth video visit with a licensed doctor 24/7 across all 50 states. Over 10 million people have already used Doctronic’s NYC‑based service to get faster, smarter, and more personal care. Skip the line. Talk to an AI Doctor Now, for free.



 Recognizing the Early Symptoms
Recognizing the Early Symptoms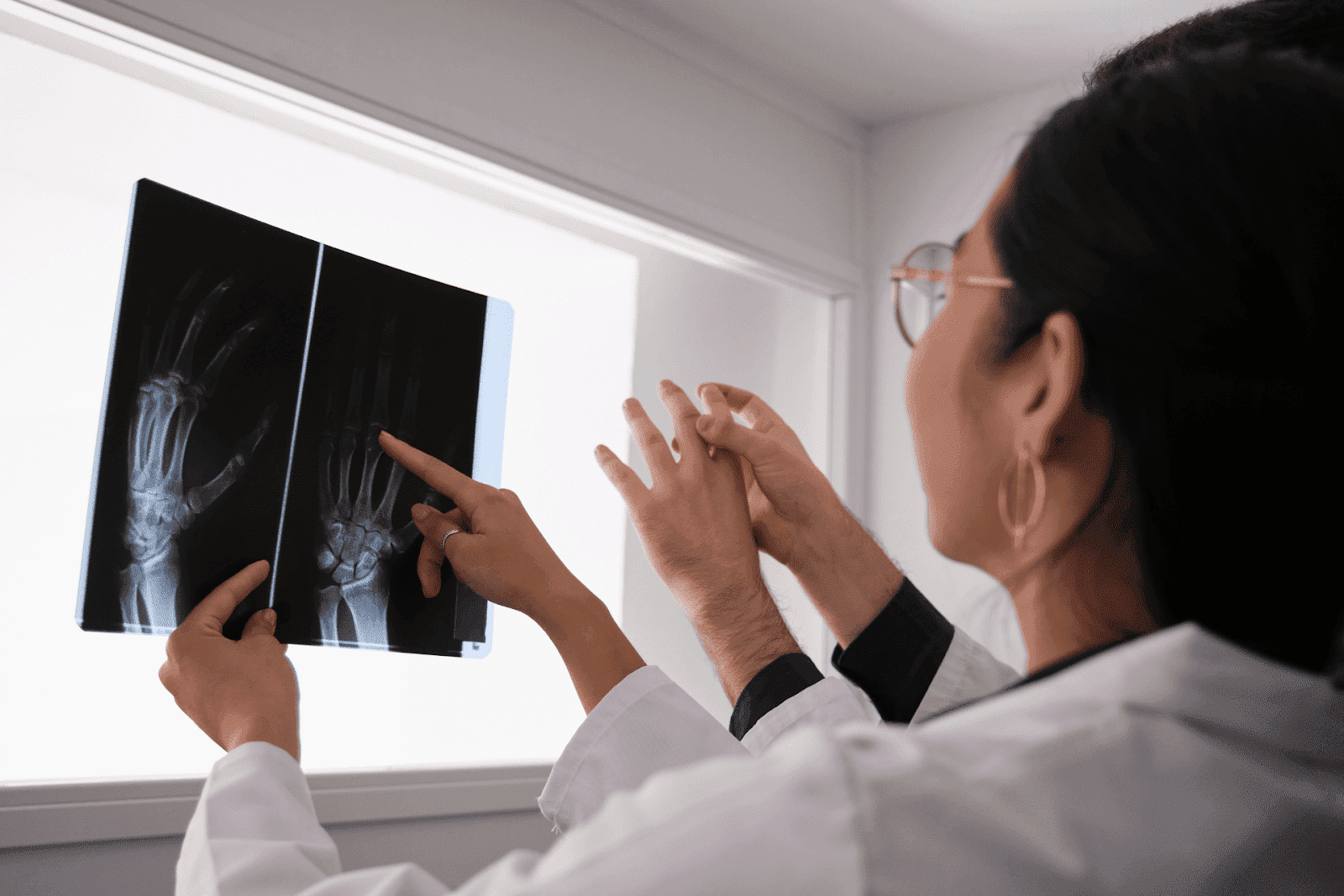 Treatment Principles: Suppress Inflammation, Prevent Damage
Treatment Principles: Suppress Inflammation, Prevent Damage