Pelvic pain can be unsettling, confusing, and sometimes frightening. It’s a symptom that spans many possible causes, from temporary muscle strain to conditions that require prompt medical attention. This guide breaks down the most common reasons for pelvic pain, what to watch for, how doctors diagnose the problem, practical self-care steps, and when to seek professional help. For convenient, affordable access to medical evaluation and follow-up, consider telehealth options like Doctronic.ai, which offers free AI doctor visits and inexpensive video visits with licensed clinicians across all 50 states.
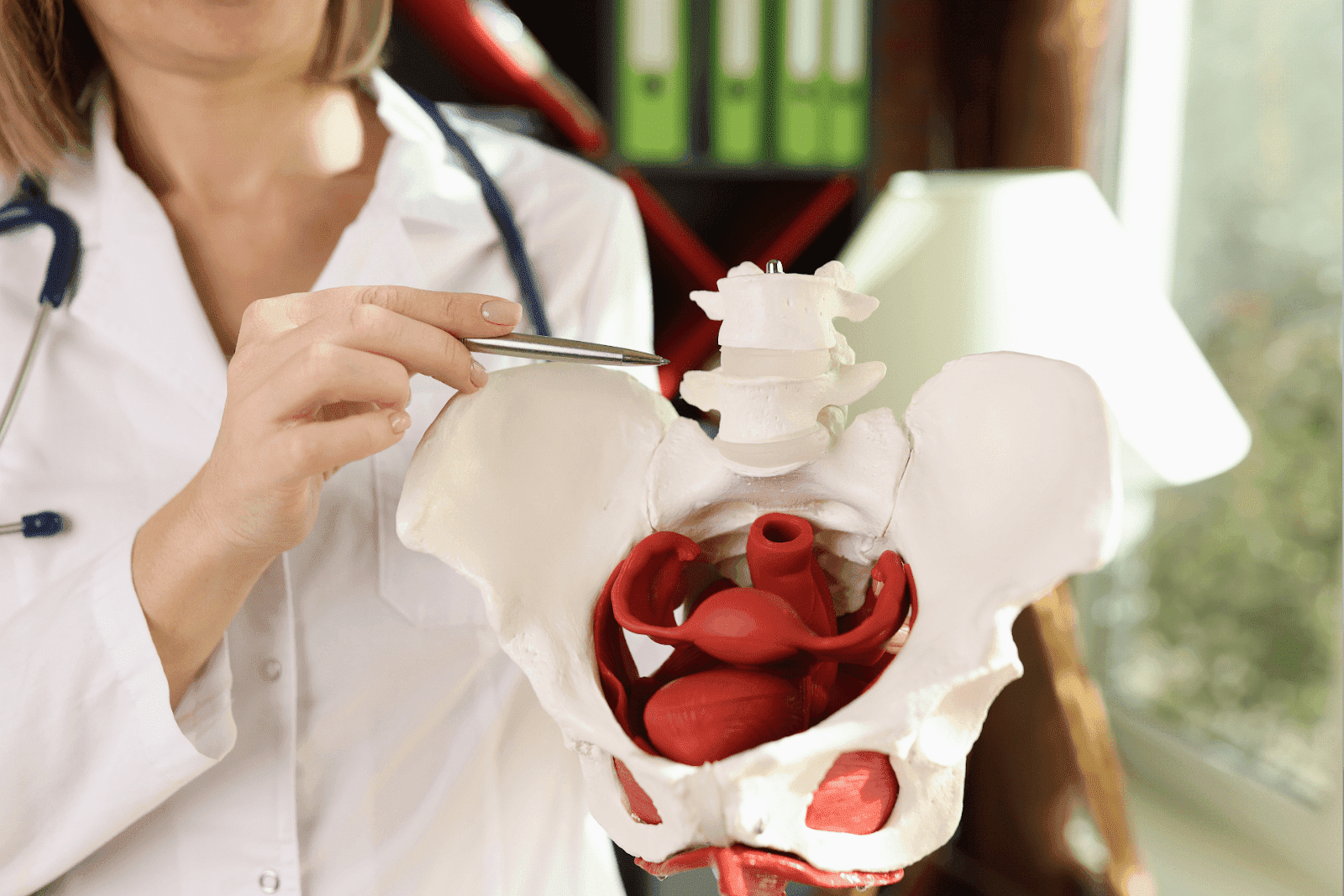
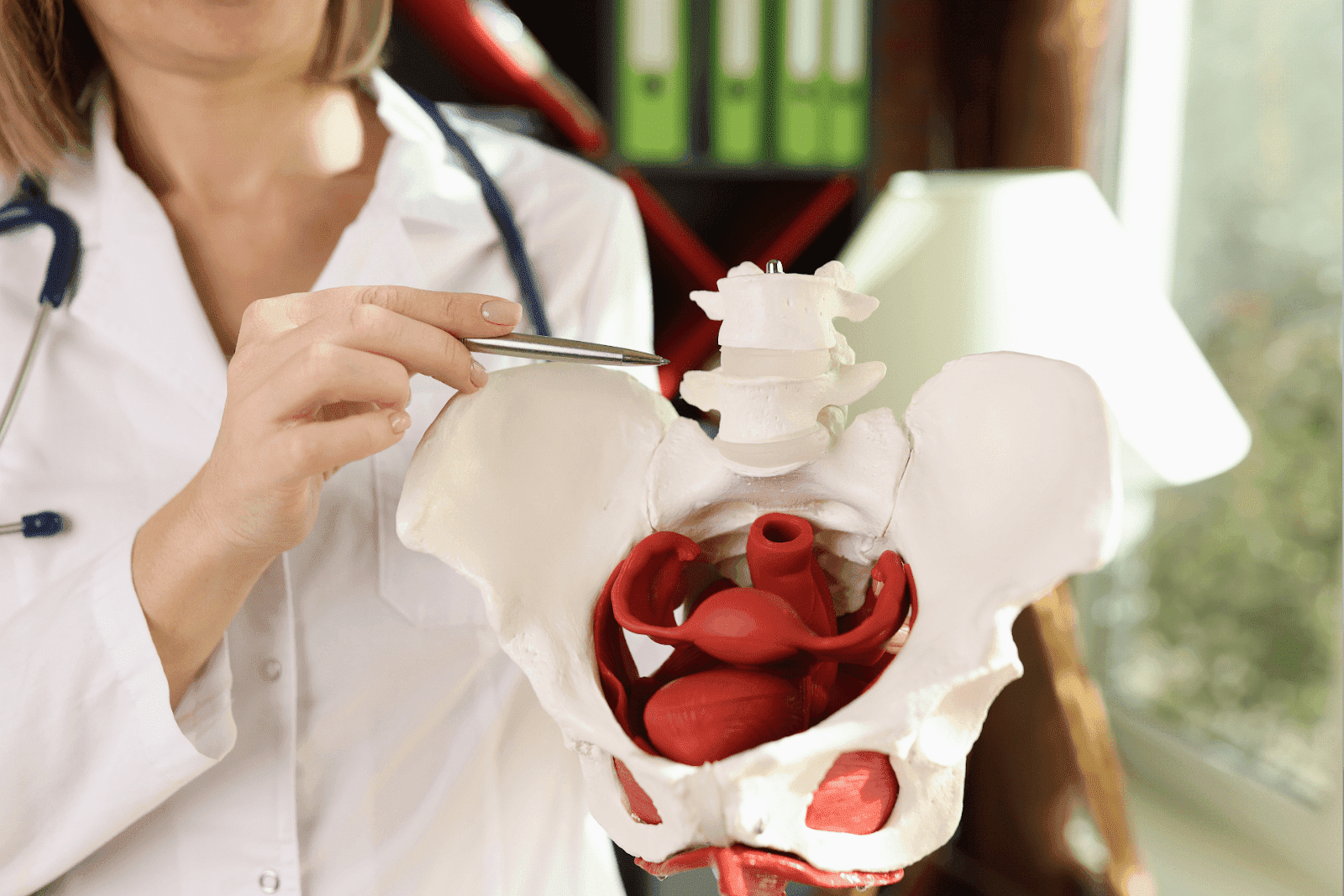
Pelvic pain can arise from many different organ systems. Common gynecologic causes include menstrual cramps, ovarian cysts, endometriosis, pelvic inflammatory disease, and complications of pregnancy such as ectopic pregnancy or miscarriage. Urologic issues like urinary tract infections, kidney stones, or interstitial cystitis can produce similar symptoms, as can gastrointestinal problems such as appendicitis, inflammatory bowel disease, diverticulitis, or constipation. Musculoskeletal sources (pelvic floor dysfunction, hernias, or sacroiliac joint pain) and neurologic conditions (nerve entrapment or neuropathic pain) are also important to consider, especially when pain is related to movement or posture.
How pelvic pain affects daily life varies widely: some people have brief episodes that respond to over-the-counter pain relief, while others experience chronic, debilitating pain that interferes with work, sleep, intimacy, and mood. Clinicians often ask about timing in relation to menstruation, bowel or bladder habits, sexual activity, prior surgeries or infections, and any change in weight or appetite to narrow the cause. Keeping a symptom diary that notes pain intensity, triggers, associated symptoms, and responses to treatments can be very helpful in guiding evaluation and management.
 Common Categories and Causes of Pelvic Pain
Common Categories and Causes of Pelvic Pain
Pelvic pain arises from several systems housed in the pelvic area. Understanding these categories helps prioritize likely causes and tests.
Gynecologic Causes
For people with female reproductive organs, gynecologic sources are among the most common causes of pelvic pain. Examples include:
Menstrual cramps (dysmenorrhea): Typical cyclical cramping around the time of the period caused by uterine contractions.
Endometriosis: When uterine lining tissue grows outside the uterus, causing chronic, often severe pain that can worsen with menstruation.
More Gynecologic Causes
Ovarian cysts: Fluid-filled sacs on the ovary that sometimes rupture or cause torsion (twisting), producing acute pain.
Pelvic inflammatory disease (PID): An infection of the reproductive organs, often due to sexually transmitted bacteria, that can cause fever, abnormal discharge, and deep pelvic pain.
Urologic Causes
Issues involving the bladder, ureters, or urethra frequently cause pelvic discomfort. Common examples:
Urinary tract infections (UTIs): Usually cause burning with urination, urinary urgency/frequency, and some lower abdominal pain.
Interstitial cystitis/bladder pain syndrome: A chronic condition presenting as persistent bladder pressure and pelvic pain without infection.
Gastrointestinal Causes
The gastrointestinal tract lies in close proximity to the pelvic organs, so bowel problems can mimic pelvic pain. Examples include:
Constipation and bowel gas: Often produce lower abdominal cramping or sharp sensations that seem pelvic in origin.
Irritable bowel syndrome (IBS): A chronic disorder of bowel function with recurrent abdominal cramping, bloating, and changes in stool pattern.
Musculoskeletal and Neuropathic Causes
Pelvic pain may arise from muscles, ligaments, pelvic floor dysfunction, or nerve entrapment, particularly after injury, childbirth, or heavy lifting.
Pelvic floor tension or myofascial pain: Tight or irritated pelvic muscles can cause deep ache and pain during sitting or sex.
Nerve-related pain: Conditions like pudendal neuralgia cause burning or shooting pain in the pelvic region.
Referred Pain and Less Common Causes
Some abdominal and systemic conditions can manifest as pelvic pain. Examples include hernias, kidney stones, appendicitis, and even some vascular conditions. Endocrine conditions, such as hormonal imbalances, can also affect menstrual-related pelvic symptoms.
Symptoms That Suggest Specific Causes
Examining the pattern of pelvic pain and accompanying symptoms often points toward the correct diagnosis. A few practical pairings to remember:
Pain with Fever or Foul Discharge
Fever with pelvic pain and abnormal vaginal discharge raises concern for pelvic inflammatory disease, tubo-ovarian abscess, or another invasive infection that may need antibiotics and urgent evaluation.
Pain with Urinary Symptoms
Burning with urination, frequency, or blood in the urine suggests a urinary tract infection, bladder inflammation, or a kidney stone.
Pain Limited to One Side
Acute, severe pain on one side could indicate ovarian torsion, a ruptured ovarian cyst, or appendicitis. These situations sometimes require immediate imaging and surgical evaluation.
Chronic, Cyclical Pain
Pain that peaks around menstrual periods, or that has lasted for months, makes endometriosis or adenomyosis more likely. Chronic pain lasting more than three months often benefits from a multidisciplinary management plan.
How Clinicians Diagnose Pelvic Pain
Diagnosis combines medical history, physical examination, laboratory tests, and sometimes imaging. The clinician’s goal is to rule out emergencies first, then identify treatable conditions.
Medical History and Physical Exam
A detailed history covers timing, character, intensity, and triggers of pain, along with menstrual, sexual, and urinary symptoms. Pelvic or abdominal examination can reveal tenderness, masses, or signs of infection.
Laboratory Tests and Cultures
Urine tests check for infection or blood. Pregnancy testing is essential in anyone capable of pregnancy with pelvic pain. Vaginal swabs and STI testing can identify infections that cause PID or cervicitis.
Imaging
Pelvic ultrasound is often the first imaging choice to evaluate the ovaries, uterus, and adnexa. CT scans are helpful if appendicitis, diverticulitis, or kidney stones are suspected. MRI can be used to assess deep endometriosis or complex pelvic pathology.
Immediate Warning Signs: When to Seek Emergency Care
Some presentations require rapid evaluation in an emergency department. Prompt assessment is critical if any of the following occur:
Sudden, severe pelvic or abdominal pain that interferes with breathing or walking.
High fever with chills and pelvic pain, especially with nausea and vomiting.
Heavy vaginal bleeding or passing large clots, fainting, or symptoms of shock (pale, clammy skin, rapid heartbeat).
Signs of pregnancy complications: severe pain with a positive pregnancy test, especially with dizziness, shoulder pain, or vaginal bleeding (possible ectopic pregnancy).
Practical Self-Care and Home Remedies
Not all pelvic pain requires medical intervention. When symptoms are mild and there are no warning signs, these self-care measures can help:
Pain Control
Over-the-counter pain relievers such as ibuprofen or acetaminophen can reduce cramp-related and inflammatory pain. Heat applied to the lower abdomen, such as heat pads or warm baths, often provides significant relief for menstrual cramps and muscle tension.
Lifestyle Adjustments
Reducing caffeine and alcohol, staying hydrated, maintaining regular bowel habits, and managing stress can improve symptoms for many people with chronic pelvic discomfort. Gentle pelvic floor stretches and guided relaxation or breathing techniques reduce muscle tension.
When to Follow Up
If symptoms persist beyond a couple of menstrual cycles, worsen, or change in character, schedule a medical evaluation. Persistent pelvic pain is not something to ignore; earlier diagnosis often leads to simpler treatment and better outcomes.
Medical Treatments and Management
Treatment depends on the underlying cause.
Infections
UTIs and pelvic infections generally require antibiotics tailored to the organism identified. Early treatment prevents complications and chronic pelvic pain.
Hormonal and Gynecologic Treatments
Hormonal contraceptives, GnRH analogs, or other hormone-based strategies can reduce menstrual-related pain and manage endometriosis symptoms. Surgical options may be recommended for certain structural problems like large fibroids, severe endometriosis, or recurrent ovarian cysts.
Physical Therapy and Pain Management
Pelvic floor physical therapy can be highly effective for musculoskeletal causes of pelvic pain. Chronic pain clinics may offer multidisciplinary care, including medications, nerve blocks, and cognitive-behavioral approaches for pain coping when needed.
 When Telehealth Makes Sense, Doctronic Can Help
When Telehealth Makes Sense, Doctronic Can Help
Telehealth is a convenient first step for many people with pelvic pain who do not have emergency warning signs. It enables rapid triage, an evidence-based evaluation, and clear guidance on whether in-person evaluation, testing, or urgent care is needed.
Doctronic.ai provides free AI-driven visits that synthesize the latest peer-reviewed medical knowledge to offer preliminary answers, treatment options, and next-step recommendations. For follow-up, affordable clinician video visits (under $40) are available 24/7 across all 50 states, making access to care seamless and timely.
What to Expect in a Telehealth Visit
During a telehealth visit, clinicians take a focused history and review symptoms closely. They can order urine tests, STI testing, pregnancy tests, or imaging if needed, and they can prescribe medications when appropriate. Telehealth is especially useful for follow-up care, medication management, and deciding who needs an urgent in-person assessment.
Common Questions People Ask About Pelvic Pain
Clear answers to frequently asked questions can reduce anxiety and help people take the right actions.
Is pelvic pain always gynecologic?
No. Pelvic pain can come from the urinary tract, bowel, muscles, nerves, or even referred pain from the back. Age, menstrual history, sexual history, and associated symptoms help narrow the likely source.
Can stress cause pelvic pain?
Stress can worsen the perception of pain and lead to pelvic floor muscle tension, which produces or intensifies pelvic discomfort. Addressing stress and mental health often improves pain outcomes.
When is pelvic pain considered chronic?
Pelvic pain typically becomes labeled chronic after persisting for three months or longer. Chronic pelvic pain often benefits from a team approach, with gynecology, urology, gastroenterology, physical therapy, and pain specialists working together.
Planning Next Steps: Questions to Ask Your Clinician
Being prepared for an appointment helps ensure a focused and productive visit. Useful questions to ask include:
What are the most likely causes of my pain based on my symptoms?
What tests are recommended and why?
Are there immediate treatments to try at home? What should prompt urgent evaluation?
If a chronic condition is diagnosed, what are the long-term management options and lifestyle changes to consider?
Understand Pelvic Pain and Take Action
Pelvic pain covers a wide spectrum of conditions, from benign menstrual cramps to serious infections or surgical emergencies. A careful history and targeted evaluation usually identify the cause. For many people, quick triage through telehealth provides reassurance and access to treatment with minimal delay. When in doubt, urgent symptoms, such as severe pain, fever, heavy bleeding, or signs of pregnancy complications, warrant immediate medical attention.
For convenient, evidence-based evaluation and ongoing care options, Doctronic’s combination of AI-guided visits and affordable clinician video visits makes it easier to get answers and start treatment quickly. Learn more or book a visit at Doctronic.ai.
Get fast, expert guidance for pelvic pain, right now
If this guide left you with questions or worrying symptoms, Doctronic can help you triage and next-step care in seconds. As the #1 AI Doctor based in NYC (now used by over 10 million people), Doctronic synthesizes the latest peer‑reviewed medical knowledge, remembers your history, and gives personalized answers instantly. Start with a free AI doctor visit on our website and, if needed, book an affordable video visit with a licensed clinician (under $40) 24/7 in all 50 states. Skip the line: Skip the line. Talk to an AI Doctor Now, for free.



 Common Categories and Causes of Pelvic Pain
Common Categories and Causes of Pelvic Pain When Telehealth Makes Sense, Doctronic Can Help
When Telehealth Makes Sense, Doctronic Can Help