A comprehensive study has demonstrated that an artificial intelligence doctor can diagnose and treat patients with accuracy matching that of experienced human physicians, showing the potential for medical AI models to assist doctors. The findings represent the first large-scale validation of a fully autonomous AI doctor operating in real-world clinical settings.
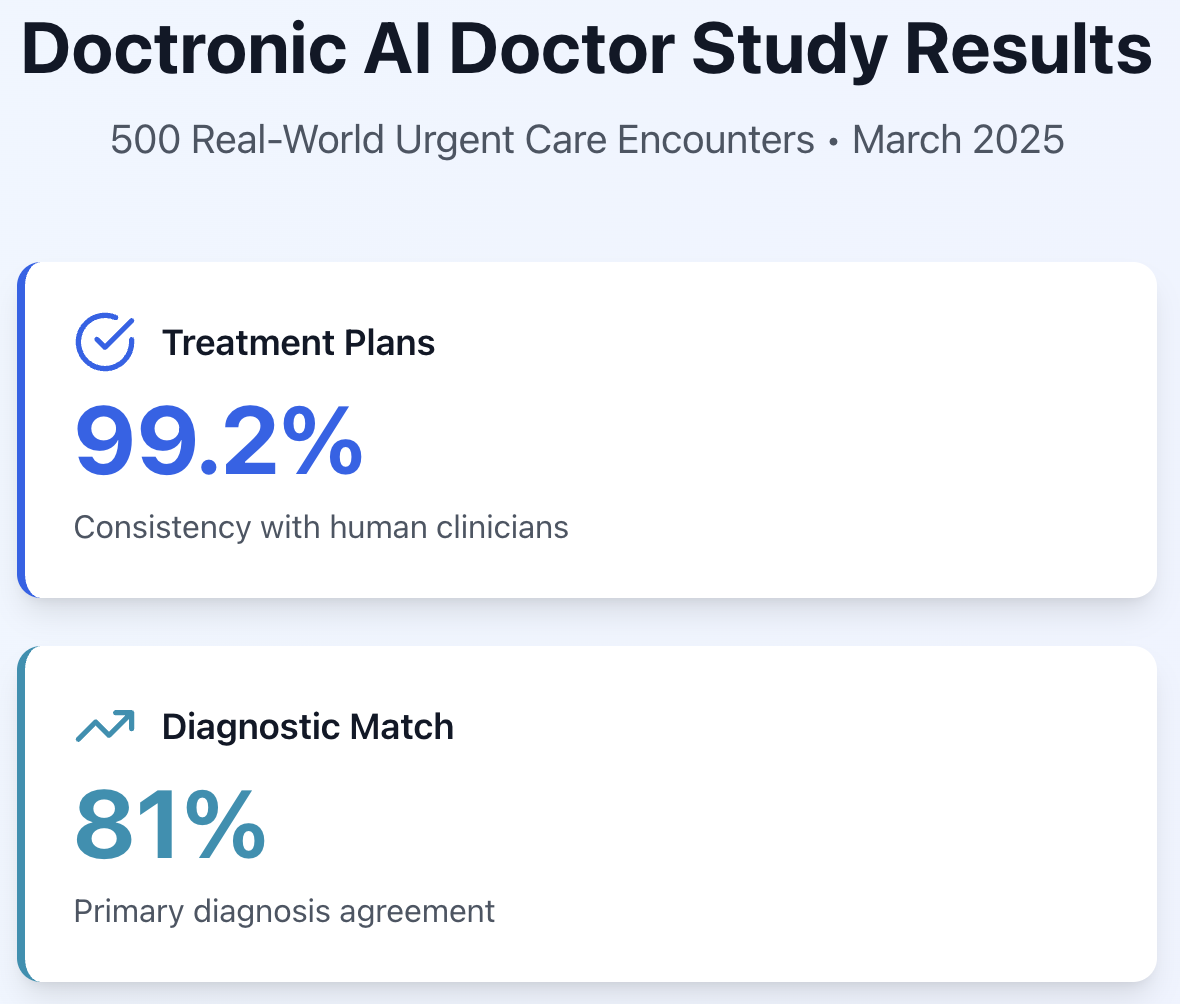
The study, conducted by the Doctronic Research Group and researchers from the University of California San Francisco, evaluated Doctronic—a sophisticated AI-powered medical system—across 500 consecutive urgent care visits. The results were remarkable: Doctronic's treatment plans aligned with those of board-certified human clinicians in 99.2% of cases, with primary diagnoses matching 81% of the time.
Perhaps most significantly, the AI system achieved zero clinical hallucinations—meaning it never invented symptoms, fabricated diagnoses, or recommended treatments unsupported by patient data. This safety record addresses one of the most significant concerns about AI in healthcare: the risk of AI "making things up."
A Healthcare Crisis Meets Technological Innovation
The timing of this breakthrough couldn't be more critical. Healthcare systems worldwide face an unprecedented workforce shortage. By 2030, the world will need an additional 11 million healthcare practitioners to meet basic health service demands—a gap that traditional solutions like medical school expansion simply cannot bridge in time.
The United States alone projects a shortage of 124,000 physicians by 2034, including 48,000 in primary care. Meanwhile, administrative burden consumes 50% of clinical time, driving burnout rates above 45% across medical specialties. Eight million lives are lost annually worldwide to treatable diseases, often because patients cannot access timely medical care.
The study aims to answer a critical question: Can artificial intelligence help solve these workforce challenges while maintaining—or even improving—the quality of patient care? The findings provide compelling evidence that the answer is yes.
How the Study Worked
Unlike previous AI medical studies that relied on hypothetical scenarios or limited test cases, this research evaluated Doctronic's performance in real-world conditions with actual patients seeking urgent medical care.
The study design was straightforward but rigorous: 500 consecutive patients visiting a virtual urgent care clinic in March 2025 first interacted with Doctronic's AI doctor, which conducted a complete medical evaluation autonomously. The same patients then met with board-certified human clinicians via video consultation. Importantly, the human doctors had access to the AI's notes but were free to conduct their own independent evaluation and reach their own conclusions.
A team of blinded evaluators—using both advanced AI evaluation tools and expert human physicians—then compared the diagnoses and treatment plans from both the AI and human doctors. The evaluators didn't know which notes came from which source, ensuring unbiased assessment.
The patient population reflected the real diversity of urgent care: people ranging from age 18 to 88, with 57% female and 42% male. They presented with over 100 different conditions spanning everything from acute sinusitis and influenza to more complex multi-system problems. More than half the patients had two or more chronic health conditions, adding realistic complexity to the diagnostic challenge.
The Results: AI Matches Human Performance
The headline findings were striking across multiple measures:
Treatment Plan Consistency: 99.2%
In 496 out of 500 cases, Doctronic and human clinicians developed treatment plans that evaluators deemed "clinically compatible"—meaning they would lead to similar therapeutic outcomes for patients. This wasn't about the AI and doctors prescribing identical medications, but rather about both arriving at appropriate, evidence-based treatment strategies.
In the four cases where treatment plans diverged, the differences were minor. For example, the AI might recommend a more comprehensive diagnostic workup for complex symptoms. Critically, none of these differences posed any risk of harm to patients.
Diagnostic Accuracy: 81% Primary Match, 95% Within Top Four
When it came to diagnosis, Doctronic's primary diagnosis matched the human clinician's in 81% of cases. When researchers expanded the comparison to include the top four most likely diagnoses from each source, agreement jumped to 95.4%.
This distinction is important because medicine often involves diagnostic uncertainty. Good doctors—whether human or AI—develop differential diagnoses: lists of possible conditions ranked by likelihood. The high agreement rate shows Doctronic consistently identified the same conditions human doctors would consider.
When AI and Doctors Disagreed: A Closer Look
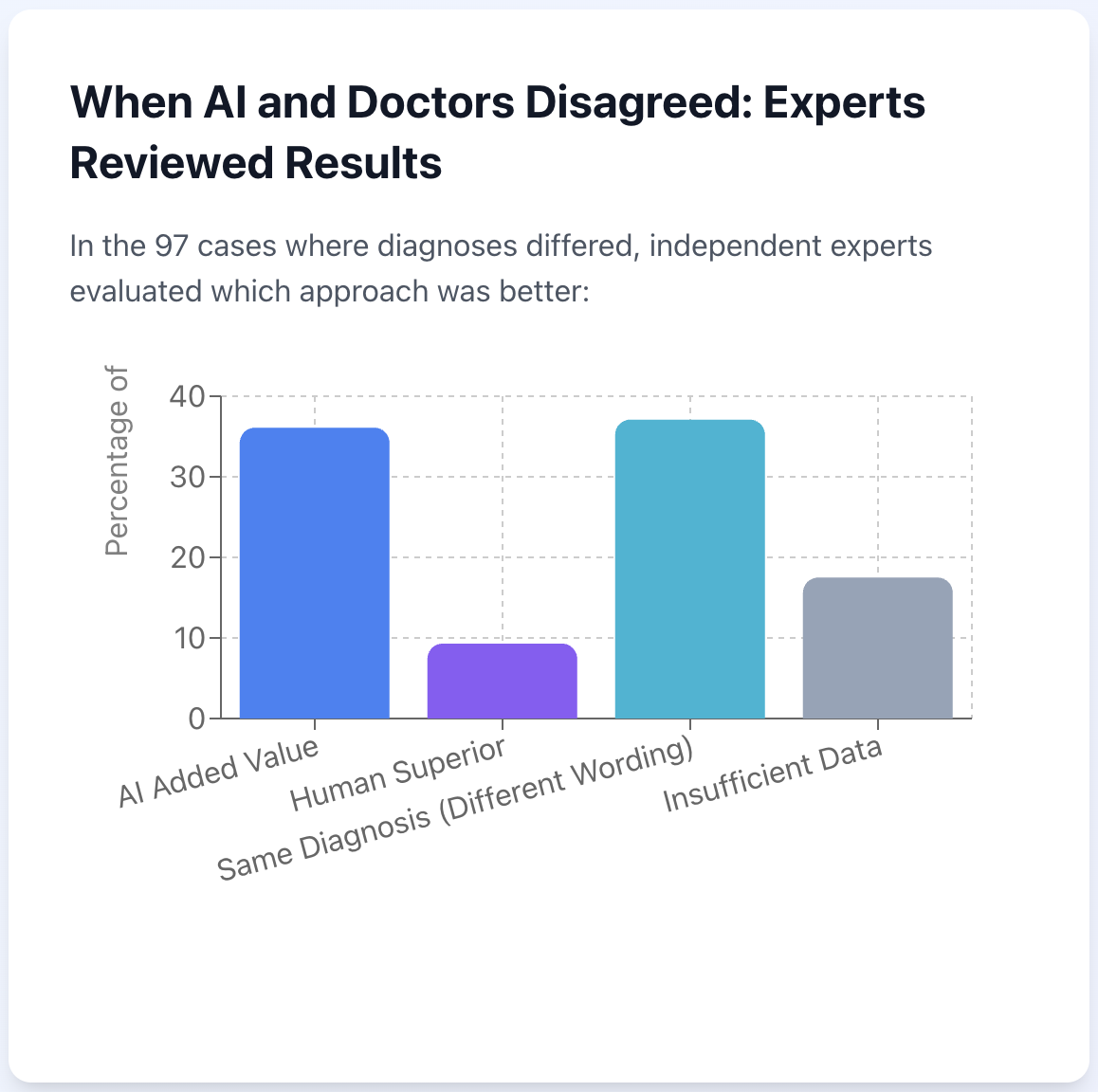
The study didn't just celebrate agreement—it carefully examined the 97 cases where the AI's primary diagnosis differed from the human clinician's. A board-certified physician manually reviewed each of these discordant cases to understand what happened.
The findings were surprising:
In 36.1% of discordant cases, the AI's clinical reasoning provided additional insights that could support the doctor's decision-making
In only 9.3% of cases was the human doctor's approach deemed better
In 37.1% of cases, the diagnoses were actually the same but worded differently (for example, "viral infection" versus "viral pharyngitis")
In 17.5% of cases, both approaches were reasonable given the available information
The cases where AI added additional value to humans typically involved conditions with clear diagnostic protocols and established guidelines—areas where AI's perfect memory of current medical literature and consistent application of best practices provided advantages. The AI also excelled at handling complex cases spanning multiple body systems, where its systematic approach helped avoid overlooking important details.
Human doctors performed better in cases involving known patterns of disease complicated by additional symptoms, where experienced clinicians felt comfortable focusing on the primary issue and documenting their reasoning for setting aside distracting symptoms.
Importantly, even in discordant cases, the AI never introduced potentially harmful errors—underscoring the robust safety mechanisms built into the system.
How Doctronic Works: The Technology Behind the Results
Doctronic represents a fundamentally different approach to medical AI. Rather than a single artificial intelligence making all decisions, Doctronic employs a "multi-agent" architecture with over 100 specialized AI components, each handling specific clinical tasks—similar to how a hospital has specialized staff for different roles.
These AI agents work cooperatively, passing information to each other dynamically as they build a complete picture of the patient's condition. The system conducts a full medical history through natural, conversational text-based chat, then generates a complete clinical note including the patient's story, physical findings, differential diagnoses, and treatment plan recommendations.
The experience for patients feels like texting with a knowledgeable doctor who asks thoughtful follow-up questions and truly listens to responses. The system draws on vast medical knowledge—current treatment guidelines, recent research, and established clinical protocols—while remembering individual patient details to provide personalized care.
Unlike general AI systems trained on internet data of uncertain quality, Doctronic was purpose-built for medicine using curated medical information and extensive safety systems to prevent the kinds of errors that would be acceptable in a chatbot but dangerous in healthcare.
What This Means for Healthcare
The implications of these findings extend far beyond one successful technology demonstration. This study establishes that autonomous AI doctors can perform at the level of experienced human physicians in urgent care settings—potentially transforming how healthcare is delivered.
Expanding Access to Care
With 11 million healthcare workers needed globally by 2030, AI doctors could help fill critical gaps. Patients in rural areas without local doctors, people needing care outside business hours, and anyone facing weeks-long wait times for appointments could receive immediate, high-quality medical evaluation.
Supporting Human Doctors
Rather than replacing physicians, systems like Doctronic can handle routine cases, allowing human doctors to focus on complex patients requiring specialized expertise, procedures that need physical presence, and situations requiring nuanced human judgment. The study found that human clinicians appreciated having AI-generated documentation to review, with one describing it as "like having the best chief resident in the world prepping them for each patient."
Reducing Healthcare Costs
AI doctors can provide care at a fraction of the cost of emergency room or urgent care visits. This economic efficiency makes quality healthcare more accessible while reducing strain on expensive healthcare resources.
Maintaining Consistent Quality
AI doesn't have bad days, doesn't get tired after long shifts, and doesn't forget important details from medical literature published last month. This consistency can help "raise the floor" of healthcare quality, ensuring all patients receive care aligned with current best practices.
Limitations and Future Directions
The researchers were careful to acknowledge limitations of their study. Most significantly, the research measured agreement between AI and human doctors—not absolute "correctness." While high agreement with board-certified clinicians is meaningful, it doesn't prove the AI is always right (nor does it prove the doctors were always right).
The study also couldn't completely avoid potential bias: human doctors saw the AI's notes before their own evaluations, potentially influencing their thinking. Additionally, the study focused on urgent care cases in English-speaking U.S. patients and evaluated single medical encounters rather than long-term patient outcomes.
A New Chapter in Healthcare
Despite limitations, this study marks a milestone in medical artificial intelligence. For the first time, researchers have demonstrated that a fully autonomous AI doctor—operating without direct human supervision—can match the diagnostic and treatment planning capabilities of board-certified physicians in real-world patient care.
The findings suggest that AI doctors aren't a distant future possibility but a present reality, capable of providing safe, effective medical care today. As healthcare systems struggle with workforce shortages and rising demand, technologies like Doctronic offer a promising path forward.
The researchers remain clear: this isn't about AI replacing human doctors. It's about expanding access to quality healthcare for millions of people who currently go without, while allowing human physicians to focus on what they do best. When a child develops strep throat at 10 PM and the nearest clinic is 40 miles away, AI doctors can help—right now, tonight.
The study's conclusion is clear: with proper design, rigorous testing, and appropriate safeguards, AI doctors can safely augment healthcare delivery, addressing critical access gaps while maintaining the quality patients deserve. For healthcare systems facing unprecedented challenges, that's not just promising research—it's a potential solution to one of society's most pressing problems.
Learn more about Doctronic and experience AI-powered healthcare at www.doctronic.ai