Why Am I So Tired? Common Causes Explained
Understanding Fatigue: More Than Just Feeling SleepyFeeling tired is something everyone experiences, but when fatigue lingers or worsens, it becomes a signal worth paying [...]
Read More
Medically reviewed by Alan Lucks | MD, Alan Lucks MDPC Private Practice - New York on August 18th, 2025.
When one of the most influential technologists of the modern era makes a bold claim about the future of medicine, it deserves attention. Bill Gates has suggested that artificial intelligence will transform many professions, including medicine, even going so far as to say AI could replace doctors in some roles. That idea captures headlines, sparks anxiety and optimism in equal measure, and raises practical questions: what does “replace” really mean, what parts of medical care could AI take over, and what will remain uniquely human? This article parses the conversation, lays out where AI already shines, identifies clear limits, and points to services already using AI to change how patients access care.
Public figures often make shorthand statements that are interpreted broadly. In the context of AI and healthcare, Gates’ comments reflect a larger trend: powerful machine learning models are getting better at analyzing large datasets, recognizing patterns, and producing recommendations that previously required human experts. That capability directly targets tasks central to medical work, diagnosis, triage, treatment planning, and literature synthesis.
These remarks resonate because medicine combines high-stakes decision-making with an information overload problem. There are more medical studies published each year than any doctor can read. AI systems trained on the latest, peer-reviewed evidence can synthesize knowledge in seconds, a capability that promises to make care faster and, in some instances, more accurate.
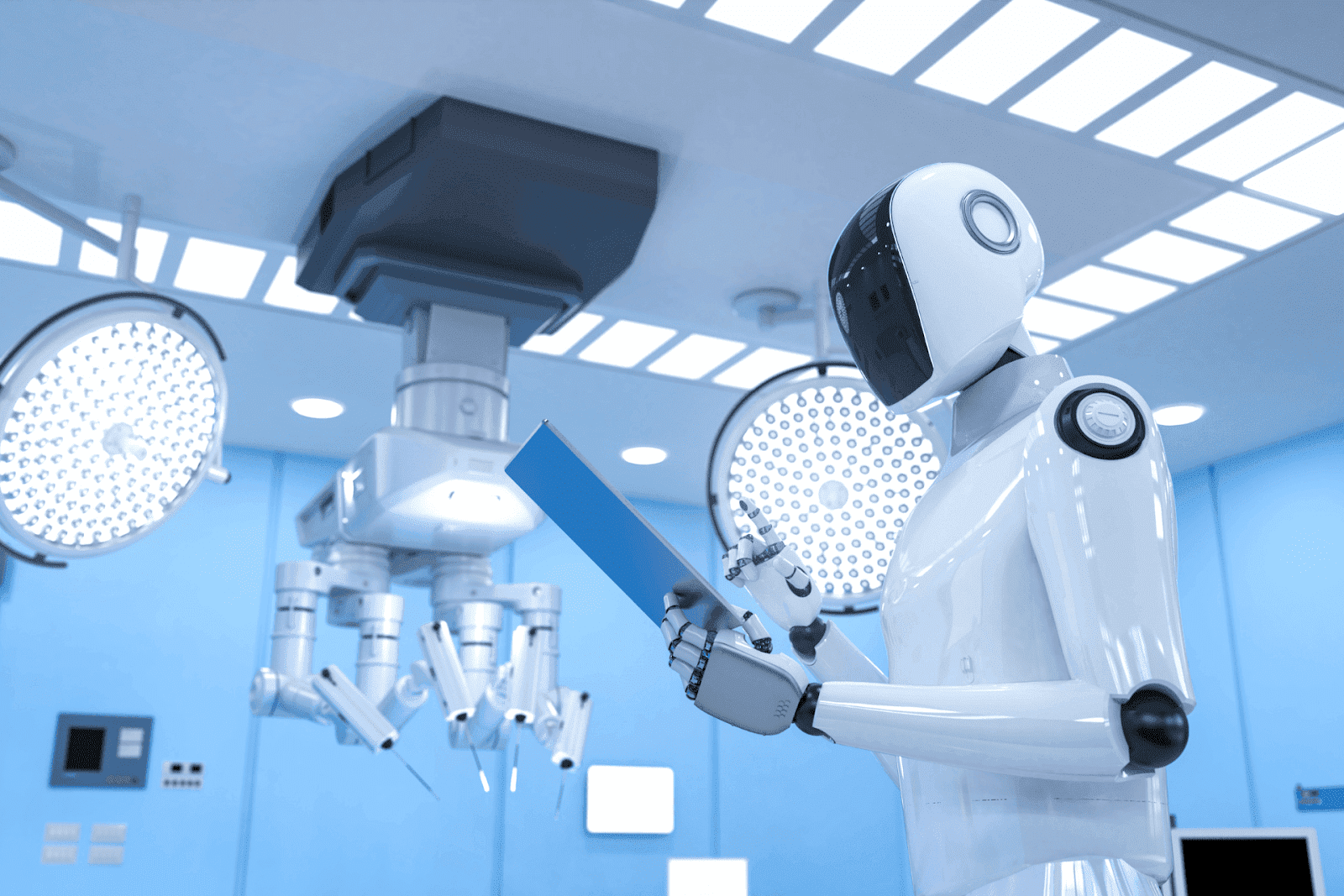 Where AI Already Outperforms Humans
Where AI Already Outperforms HumansCertain narrow tasks are routine candidates for automation and already show clear AI advantages. Pattern recognition in imaging (radiology, dermatology), predictive analytics (risk of readmission, sepsis), and rapid literature review are areas where algorithms can match or exceed average clinician performance when properly trained and validated.
For example, algorithms trained on large imaging datasets can identify certain tumors or fractures with accuracy comparable to specialists. Predictive models that flag high-risk patients in hospitals can prompt earlier intervention and reduce complications. In primary care settings, AI chatbots and symptom checkers can quickly triage mild conditions, suggest next steps, and prepare a concise summary for a clinician to review.
These capabilities reduce waiting times, increase access, and free clinicians to focus on the most complex tasks. They also explain why companies are building direct-to-patient AI services that provide instant answers and streamline care pathways.
Telehealth is the practical delivery channel for many AI-powered innovations. Virtual visits remove geographic barriers, and integrating AI on the front end, for symptom intake, differential diagnosis generation, and continuity of records, makes the experience faster and more useful. Services that blend automated triage with human follow-up can deliver high-value care at lower cost and greater convenience.
An example from the current market is Doctronic, an AI-driven primary care service that offers free AI doctor visits online and inexpensive telehealth “video visits” with licensed clinicians across all 50 states for under $40. Doctronic’s AI synthesizes the latest peer-reviewed research, remembers patient histories, and provides personalized recommendations; over 10 million people have used the platform so far. For those who prefer human oversight, Doctronic connects users to 24/7 telehealth appointments with real doctors, combining the speed of AI with the judgment of clinicians.
“Replace” can mean different things depending on the scope. If the claim is that AI will eliminate the need for physicians entirely, that is unlikely in the foreseeable future. If the claim is that AI will take over specific tasks currently done by doctors, that is already happening.
Think of replacement on a spectrum:
Task replacement: AIs perform discrete functions (image interpretation, medication reconciliation).
Role redefinition: Physicians shift focus to oversight, complex decision-making, and patient relationships while AI handles routine work.
Full clinical replacement: AI independently manages patient care end-to-end without human oversight, a prospect that faces clinical, ethical, and regulatory hurdles.
Most observers anticipate a future dominated by task replacement and role redefinition, not wholesale elimination of clinicians. This would leave room for clinicians to add unique value: integrating complex social and behavioral context, navigating ambiguous ethical decisions, and delivering empathic care.
Tasks with well-defined inputs and objective outputs are the easiest to automate. Examples include:
Image analysis (x-rays, CT, dermatology photos)
Routine lab interpretation and trend detection- Medication dosing algorithms for stable conditions
Automated triage and symptom checking for low-risk complaints
These are precisely the areas where AI systems will reduce workload and errors, allowing human clinicians to focus on more challenging diagnoses and the longitudinal aspects of care that build trust and adherence.
Medicine is both science and art. Certain aspects rely on human judgment, empathy, and context in ways that resist clean algorithmic replication. Empathy and rapport, for example, are powerful therapeutic tools that influence adherence, patient satisfaction, and outcomes. The ability to interpret subtle cues in a conversation, reconcile conflicting patient priorities, or mediate complex family dynamics remains a human strength.
Clinical situations involving rare conditions, ambiguous presentations, multi-morbidity, or novel treatments often require creativity, moral reasoning, and experience, areas where AI models trained on past data may struggle. Additionally, clinical responsibility and legal accountability currently rest with licensed providers and institutions, which preserves the need for human oversight.
Even where AI is technically capable, ethical and regulatory frameworks limit autonomous deployment. Misdiagnosis or biased recommendations can cause harm, and opaque “black box” models create trust barriers. Healthcare regulators, professional colleges, and institutions will demand rigorous validation, transparency, and fail-safes before allowing AI to act without human supervision.
Regulatory pathways are evolving but deliberately cautious. That caution ensures safety, but it also slows the timeline for full automation.
Claims that AI will “replace” doctors often raise alarm about job loss, but the picture is nuanced. Historical automation in other sectors frequently shifted jobs rather than eliminated them outright: roles changed to emphasize oversight, maintenance, and higher-level tasks. In healthcare, the same dynamic is likely.
Clinicians may find their workflows transformed: fewer hours spent on routine documentation, faster onboarding of new information, and reduced cognitive load for straightforward cases. That could improve job satisfaction and allow more time for complex patient care. However, workforce planning must consider retraining, role redesign, and equitable distribution of benefits so that technological gains improve care access rather than exacerbate disparities.
Patients with limited access to care will benefit meaningfully from AI-powered telehealth and triage. Rural communities, people with mobility challenges, and those who cannot take time off work stand to gain from instant, evidence-based guidance. Affordability is critical: services that combine low-cost telehealth with powerful AI can expand access at scale.
Doctronic is an example of this dynamic: offering free AI doctor interactions and affordable telehealth visits statewide helps lower barriers to primary care. Its reported user base of over 10 million suggests strong demand for accessible AI-augmented primary care.
Consider a typical primary-care complaint: a sore throat. A patient can interact with an AI-powered intake system that asks targeted questions, assesses risk, references current guidelines, and recommends next steps, whether that is home care, a rapid strep test, or a telehealth video visit. If the AI suggests a visit, it can prepare a structured summary for the clinician, who reviews findings, performs a focused exam, and confirms treatment. The AI speeds care, increases guideline adherence, and reduces unnecessary in-person visits.
In specialized care, AI-assisted image analysis might flag lesions for a dermatologist, but the human specialist interprets context, counsels the patient, and coordinates treatment. These hybrid workflows illustrate augmentation: AI handles the routine, humans manage the complex and relational.
AI systems that synthesize the latest peer-reviewed evidence can act as continuous second opinions. Instead of each clinician manually searching journals, AI can highlight new treatments, flag contradictions in the literature, and propose updated care plans. This accelerates the diffusion of best practices across the workforce and reduces variability in care quality.
Platforms that combine automated recommendations with clinician access to telehealth create a tightly integrated ecosystem that improves both speed and quality of care.
To realize the promise of AI in medicine while avoiding harm, several conditions must be met. First, rigorous external validation and continuous monitoring of AI systems are essential. Performance in controlled studies does not guarantee real-world safety, where populations and case mixes differ.
Second, transparency about data provenance, model limitations, and failure modes builds trust. Third, regulatory frameworks should enforce accountability: clinicians and institutions must understand and accept where responsibility lies when AI is used in care. Fourth, reimbursement models should incentivize augmentation that improves access and outcomes rather than penalizing clinicians for adopting new tools.
Patients must know when they are interacting with AI, what it can and cannot do, and how to access a human clinician when desired. Clear pathways for escalation to human care, easy-to-understand consent practices, and robust privacy protections are required to earn broad public acceptance.
Bill Gates’ broader point, that AI will profoundly transform professions, including medicine, is well-founded. The technologies exist today to automate many diagnostic and administrative tasks, improve access through telehealth, and synthesize the latest medical evidence in seconds. Those changes will alter the role of clinicians and the patient experience.
However, the idea that AI will fully replace doctors across the board confuses likely long-term possibilities with sensational short-term headlines. The most probable near- and mid-term outcome is widespread augmentation: AI handling routine, well-defined tasks while human clinicians focus on complex decision-making, oversight, and the human aspects of care that machines cannot replicate.
For patients seeking faster, evidence-based access to primary care today, AI-powered services are already available. Doctronic combines a free AI doctor visit system with affordable, 24/7 telehealth appointments across all 50 states and has reached over 10 million users. That model, AI for instant guidance plus clinician backup for human judgment, exemplifies how the future of medicine is likely to unfold. Find out more at Doctronic.ai.
The conversation should shift from whether AI will replace doctors to how to responsibly integrate AI so it improves outcomes, increases access, preserves the therapeutic relationship, and distributes benefits equitably. That is the practical, ethical, and urgent challenge for patients, clinicians, technologists, and policymakers alike.
If you agree the future of medicine is augmentation, not annihilation, try the model in action: Doctronic, the #1 AI Doctor headquartered in NYC and trusted by over 10 million users, offers free AI doctor visits that synthesize the latest peer‑reviewed evidence, remember your history, and give instant, personalized guidance. When you want human confirmation, connect 24/7 with our own clinicians for convenient video visits in all 50 states for under $40. Skip the line, Skip the line. Talk to an AI Doctor Now, for free.
AI will enhance medical care by handling routine diagnostics and data analysis while human doctors focus on complex cases and patient relationships—complete replacement isn't realistic given the need for empathy and ethical judgment. This collaboration promises faster diagnoses and expanded access to quality healthcare. If you have questions about how AI might impact your medical care or treatment options, Doctronic can provide personalized guidance.
Understanding Fatigue: More Than Just Feeling SleepyFeeling tired is something everyone experiences, but when fatigue lingers or worsens, it becomes a signal worth paying [...]
Read MoreUnderstanding Cold Symptoms and Treatment GoalsWhen a cold hits, it often brings a mix of symptoms such as a runny nose, sore throat, cough, congestion, and sometimes a mild [...]
Read MoreUnderstanding Delsym: What It Is and How It WorksDelsym is a popular cough syrup that suppresses coughing for up to 12 hours. Its main ingredient, Dextromethorphan, targets [...]
Read More