Swollen lymph nodes, often felt as tender lumps under the jaw, in the neck, armpits, or groin, are a common reason people worry and search for answers. While they usually signal the immune system doing its job, there are times when swollen nodes warrant prompt medical evaluation. This article explains what causes lymph node swelling, which signs suggest a more serious problem, how clinicians evaluate enlarged nodes, and practical next steps for care, including convenient telehealth options like Doctronic.ai.
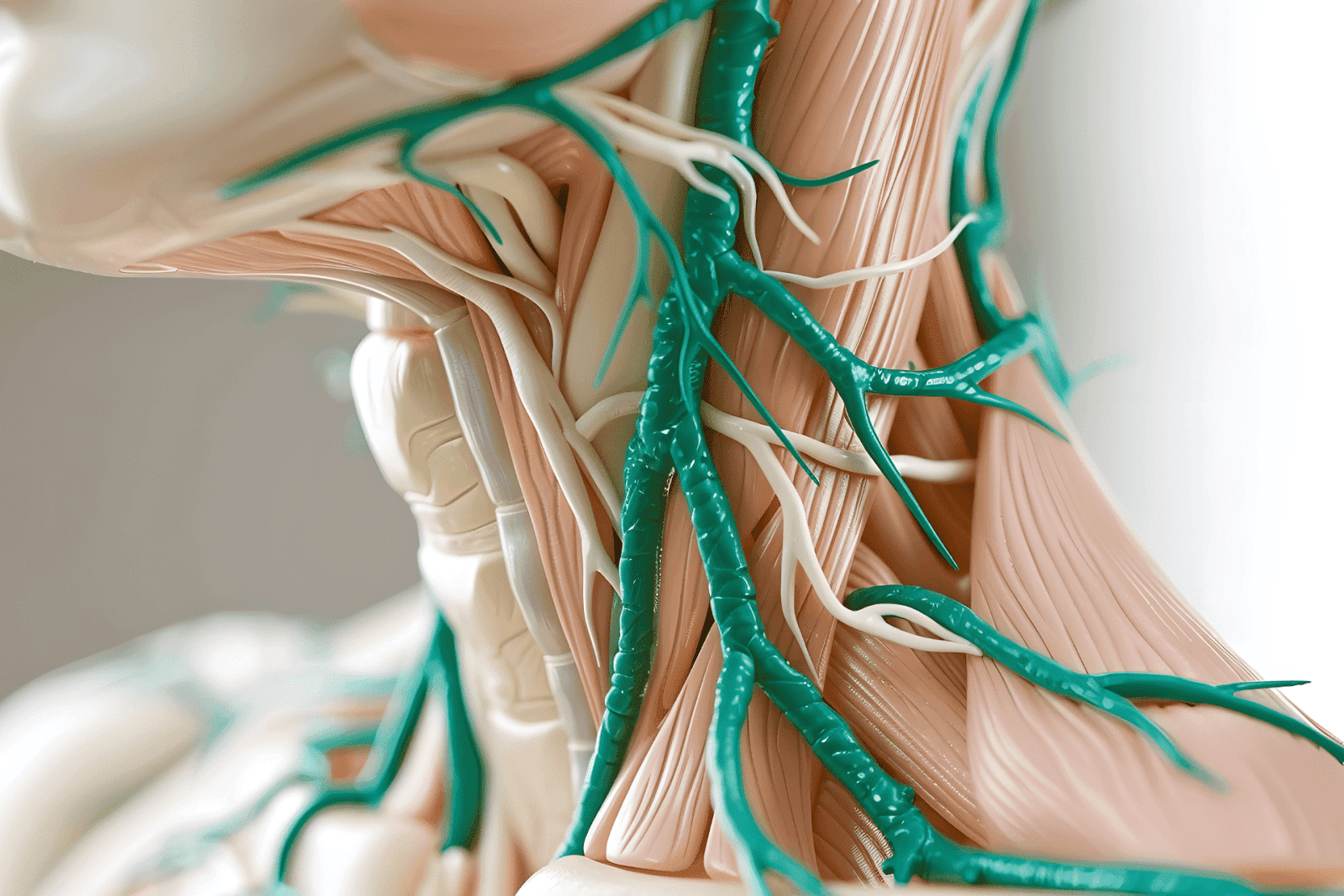
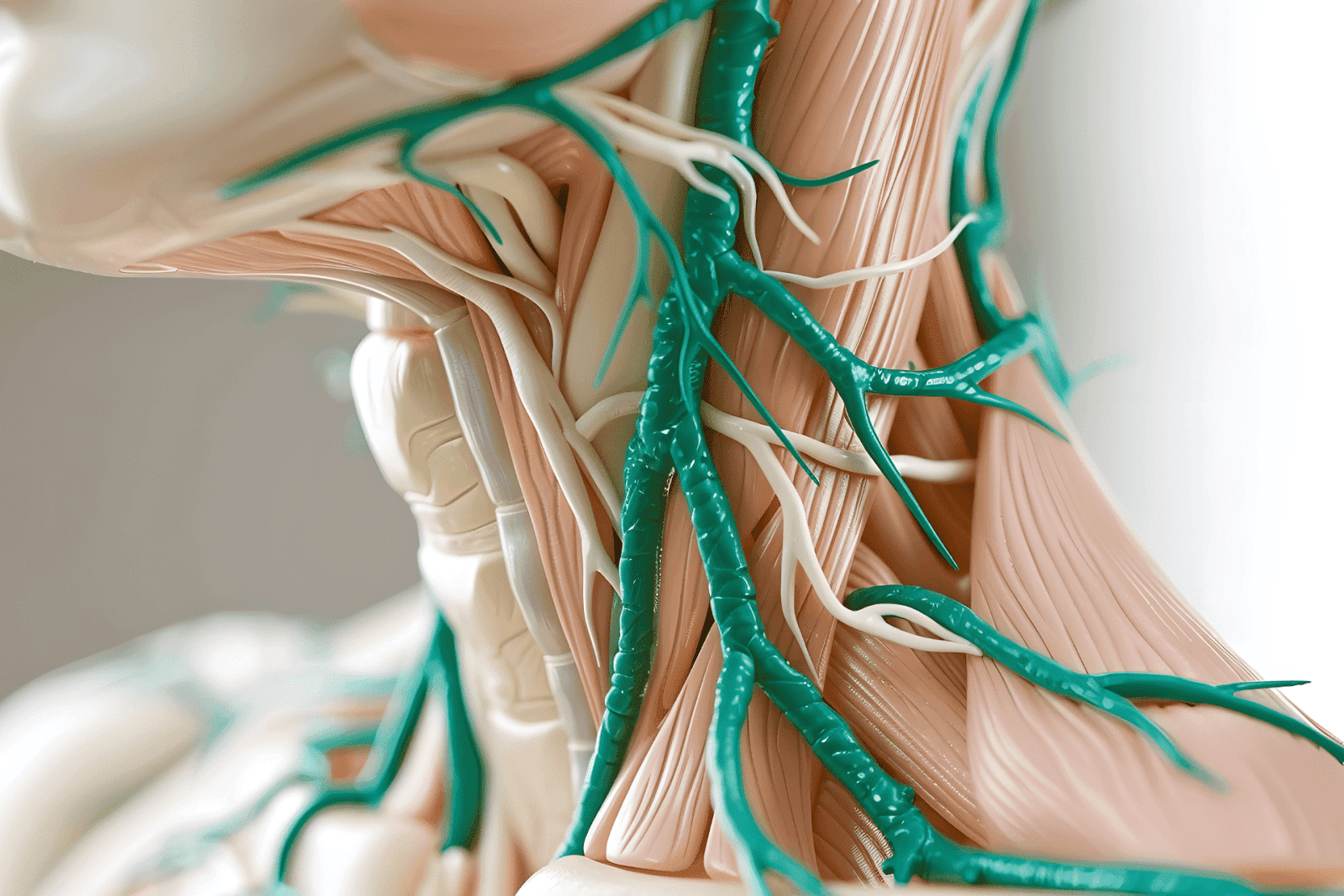
What Are Lymph Nodes and Why Do They Swell?
Lymph nodes are small, bean-shaped organs scattered throughout the body. They act as filters for lymphatic fluid and as hubs where immune cells meet invading organisms or abnormal cells. When immune cells mount a response, lymph nodes can increase in size due to a surge of immune activity, inflammation, or the proliferation of cells within the node.
Common reasons for swelling include infections (viral or bacterial), localized skin or soft tissue infections, immune system activation from autoimmune conditions, and, less commonly, malignancies such as lymphoma or metastatic cancer. Location matters: for example, nodes near the throat often swell with upper respiratory infections, while groin nodes may respond to lower extremity infections.
 Typical Causes of Swollen Lymph Nodes
Typical Causes of Swollen Lymph Nodes
Most swollen nodes are benign and related to infections. Some of the typical causes include:
Viral infections: common cold, influenza, mononucleosis, and COVID-19.
Bacterial infections: strep throat, infected cuts, or skin infections like cellulitis.
Localized infections: ear infections, dental abscesses, or sinusitis.
Systemic infections: HIV, tuberculosis, and certain tropical infections, depending on travel history.
Immune conditions: lupus, rheumatoid arthritis, and other autoimmune diseases.
Cancer: Hodgkin and non-Hodgkin lymphoma, and cancers that metastasize to lymph nodes.
Medications and inflammatory reactions: Certain drugs can cause generalized lymphadenopathy as a side effect.
Which Features Suggest a Benign Cause?
Several characteristics point toward reactive (benign) lymph node enlargement:
Red flags for likely benign causes include tenderness to touch, soft or rubbery texture, and mobility (the node moves slightly under the skin). Nodes that enlarge rapidly in the context of recent infection or that diminish over days to weeks as symptoms resolve usually reflect the immune system doing its job.
When Size Alone Isn’t Enough
Size matters somewhat; adult lymph nodes larger than 1–2 centimeters may warrant attention, but the context is crucial. A 2.5 cm tender, fluctuant node near a skin boil likely represents an abscess and can be managed conservatively or drained if indicated. Conversely, a firm, fixed 1.5 cm node without pain might prompt further evaluation to rule out malignancy.
When Swollen Lymph Nodes Are Concerning
Most swollen lymph nodes resolve on their own, but certain symptoms should prompt medical evaluation. Seek care if any of the following are present:
Persistent enlargement for more than 2–4 weeks without improvement.
Nodes that are hard, fixed to underlying tissues, or progressively enlarging.
Associated systemic symptoms such as unexplained fever, night sweats, unintentional weight loss, or persistent fatigue.
Difficulty breathing, swallowing, or speaking if the swelling is in the neck or chest area.
Redness, warmth, or severe pain suggesting an abscess or cellulitis.
Recent history of unexplained travel, tick bites, or high-risk exposures that raise suspicion for specific infections.
Red Flags That Require Urgent Attention
Immediate evaluation is needed if the swelling is accompanied by high fever, rapidly progressive enlargement, signs of airway compromise, or severe local infection that could spread. In those situations, in-person assessment and possibly urgent imaging or surgical drainage might be necessary.
How Clinicians Evaluate Swollen Lymph Nodes
The medical evaluation typically begins with a focused history and physical exam. Important history elements include duration of swelling, recent infections, travel history, animal or tick exposures, recent vaccinations, medications, and systemic symptoms.
On exam, clinicians assess size, tenderness, consistency (soft, rubbery, firm), mobility, and whether the enlargement is localized or generalized. Location provides clues; for example, supraclavicular nodes, above the collarbone, are more suggestive of intra-thoracic or intra-abdominal pathology and are evaluated more aggressively.
Common Diagnostic Tests
Depending on the clinical picture, clinicians may order:
Blood tests: complete blood count, markers of inflammation (CRP, ESR), and specific serologies for infections such as EBV (mononucleosis), HIV, or syphilis.
Imaging: ultrasound is a useful first test for superficial nodes to characterize size, internal architecture, and the presence of fluid. CT or MRI may be used for deeper or more concerning findings.
Biopsy: fine-needle aspiration or core needle biopsy can provide tissue for cytology and culture. Excisional biopsy is sometimes required when lymphoma is suspected.
Treatment Options Based on Cause
Treatment for swollen lymph nodes depends entirely on the underlying cause. When an infection is identified as the trigger, targeted therapy is used. For example, bacterial infections may require antibiotics, while viral illnesses usually need supportive care.
For inflammatory or autoimmune conditions, treatment targets the underlying disease with immunomodulatory medications. If malignancy is diagnosed, oncology-directed therapy is initiated based on the specific cancer type and stage.
Self-Care and Symptom Relief
Simple measures can help alleviate discomfort while the underlying cause is addressed:
Warm compresses applied to the area for 10–15 minutes several times a day can reduce pain and promote drainage for inflamed nodes.
Over-the-counter pain relievers like acetaminophen or NSAIDs (ibuprofen) can relieve fever and tenderness when not contraindicated.
Good hydration, rest, and treating any local source of infection (dental care, skin wounds) support recovery.
When to Use Telehealth and How It Helps
Telehealth is an excellent first step for non-urgent concerns about swollen lymph nodes. A virtual visit allows a clinician to triage symptoms, review history, guide self-exam techniques, and determine whether tests or in-person care are necessary. Telehealth also offers fast access to care and can save time and travel, especially helpful when nodes are painful but there are no red-flag symptoms.
Doctronic.ai offers both free AI-driven visits and convenient telehealth video visits with licensed clinicians for under $40, available 24/7 across all 50 states. The platform combines an AI “doctor” that synthesizes the latest, peer-reviewed medical research with human clinicians who can provide video consultations and arrange tests or referrals when needed. With over 10 million people already using the system, Doctronic is positioned as a fast, modern option for initial assessment.
What to Expect During a Telehealth Visit
During a telehealth appointment, a clinician will take a focused history and ask the patient to describe the location, size, tenderness, onset, and progression of the swelling. The clinician may guide a self-exam to palpate the node and assess the surrounding skin. Based on the findings, the clinician can recommend blood tests, arrange imaging, prescribe antibiotics if bacterial infection is likely, or advise an in-person biopsy if cancer is suspected.
When immediate in-person care is not required, telehealth can provide reassurance, symptom management, and a structured plan for follow-up. For those who prefer to combine AI and human expertise, Doctronic.ai offers rapid AI-driven answers and low-cost video visits with human doctors, enabling personalized and continuous care. The AI “remembers” prior interactions to provide more contextually aware guidance.
Special Situations and Vulnerable Groups
Children frequently develop swollen lymph nodes with routine infections. Pediatric nodes can be reactive and benign, but persistent or unusual features require pediatric evaluation. Newborns and infants with enlarged nodes should be seen promptly because their immune systems and symptom patterns differ from those of adults.
People with weakened immune systems, whether due to medications (like chemotherapy or long-term steroids), HIV, or organ transplantation, have a higher risk that swollen nodes reflect severe or atypical infections and should be evaluated more quickly. Similarly, older adults and those with a personal history of cancer may need an expedited workup for possible malignancy.
Travel History and Exposures
Travel to areas with endemic infections (e.g., tuberculosis, certain parasitic diseases) or exposure to animals or ticks can change the differential diagnosis. Always inform clinicians about recent travel, insect bites, or contact with animals during the initial evaluation because that information guides appropriate testing and empiric treatment decisions.
What to Expect from Follow-Up and Monitoring
Follow-up is often tailored to the suspected cause. If lymph node swelling is clearly linked to a transient infection and symptoms are improving, clinicians may recommend watchful waiting with re-evaluation in 2–4 weeks. Persistent or enlarging nodes trigger further testing, such as imaging or biopsy.
For diagnosed conditions like lymphoma or chronic infection, a long-term care plan with specialists may be needed. Communication and continuity of care are essential; platforms that maintain a comprehensive record of prior visits and findings can improve care coordination and reduce repeated testing.
Practical Checklist: When to See a Clinician in Person
Use this simple checklist to decide whether to schedule an in-person visit:
Red flags present (high fever, airway compromise, rapidly growing mass).
No improvement after 2–4 weeks or progressive enlargement.
Hard, fixed, or painless nodes without a clear infection source.
Concerning systemic symptoms (night sweats, weight loss, prolonged fatigue).
High-risk status (immunosuppression, prior cancer, unusual exposures).
If none of these apply but uncertainty remains, starting with a telehealth visit can provide fast triage and next-step recommendations without delay.
 Frequently Asked Questions (FAQ)
Frequently Asked Questions (FAQ)
How Long Do Swollen Lymph Nodes Usually Last?
When caused by a common viral infection, lymph nodes typically start to shrink within a week and often resolve within 2–4 weeks. Bacterial infections treated with antibiotics may improve more quickly once appropriate therapy begins. Persistent nodes beyond a month merit medical follow-up.
Can Stress or Lack of Sleep Cause Swollen Lymph Nodes?
Stress and poor sleep do not directly cause lymph node enlargement. However, chronic stress can weaken immune defenses and increase susceptibility to infection, which may indirectly lead to swollen nodes.
Are Painful Nodes Always Infected?
Painful, tender lymph nodes commonly reflect inflammatory or infectious causes. Painless enlargement can be more concerning for malignancy, but this is not absolute. Clinical context determines the next steps.
Bottom Line and Next Steps
Swollen lymph nodes are common and most often harmless, reflecting a working immune system. Attention should focus on duration, associated symptoms, node characteristics, and the overall clinical context. Red flags such as rapid growth, fixation, systemic symptoms, or airway compromise require prompt evaluation.
Telehealth provides a fast, effective way to triage swollen lymph nodes and determine whether in-person tests or treatments are needed. For accessible, modern care options that combine AI-driven assessment and affordable video visits with human clinicians, Doctronic.ai is a useful resource for initial evaluation and follow-up. With more than 10 million users and 24/7 telehealth availability in all 50 states, Doctronic aims to deliver quick, evidence-based guidance grounded in up-to-date medical research.
Need Fast, Reliable Guidance About Swollen Lymph Nodes?
If you’re unsure whether a lump needs urgent care, try Doctronic, the #1 AI Doctor based in NYC that over 10 million people trust. Our AI-driven visits are free, synthesize the latest peer‑reviewed medical evidence, remember your history, and can quickly tell you whether to watch and wait or see a clinician. When you want a human, our licensed doctors offer convenient video visits for under $40, 24/7 in all 50 states. Skip the line. Talk to an AI Doctor Now, for free.



 Typical Causes of Swollen Lymph Nodes
Typical Causes of Swollen Lymph Nodes Frequently Asked Questions (FAQ)
Frequently Asked Questions (FAQ)