Digestive discomfort is a common complaint that many people experience at some point in their lives. While occasional indigestion or bloating might be harmless, persistent digestive issues could signal a more serious underlying condition. One such condition that often goes undiagnosed is Exocrine Pancreatic Insufficiency (EPI). If you’ve been struggling with digestion and haven’t found relief, understanding EPI and its symptoms could be the key to better health.
What Is Exocrine Pancreatic Insufficiency (EPI)?
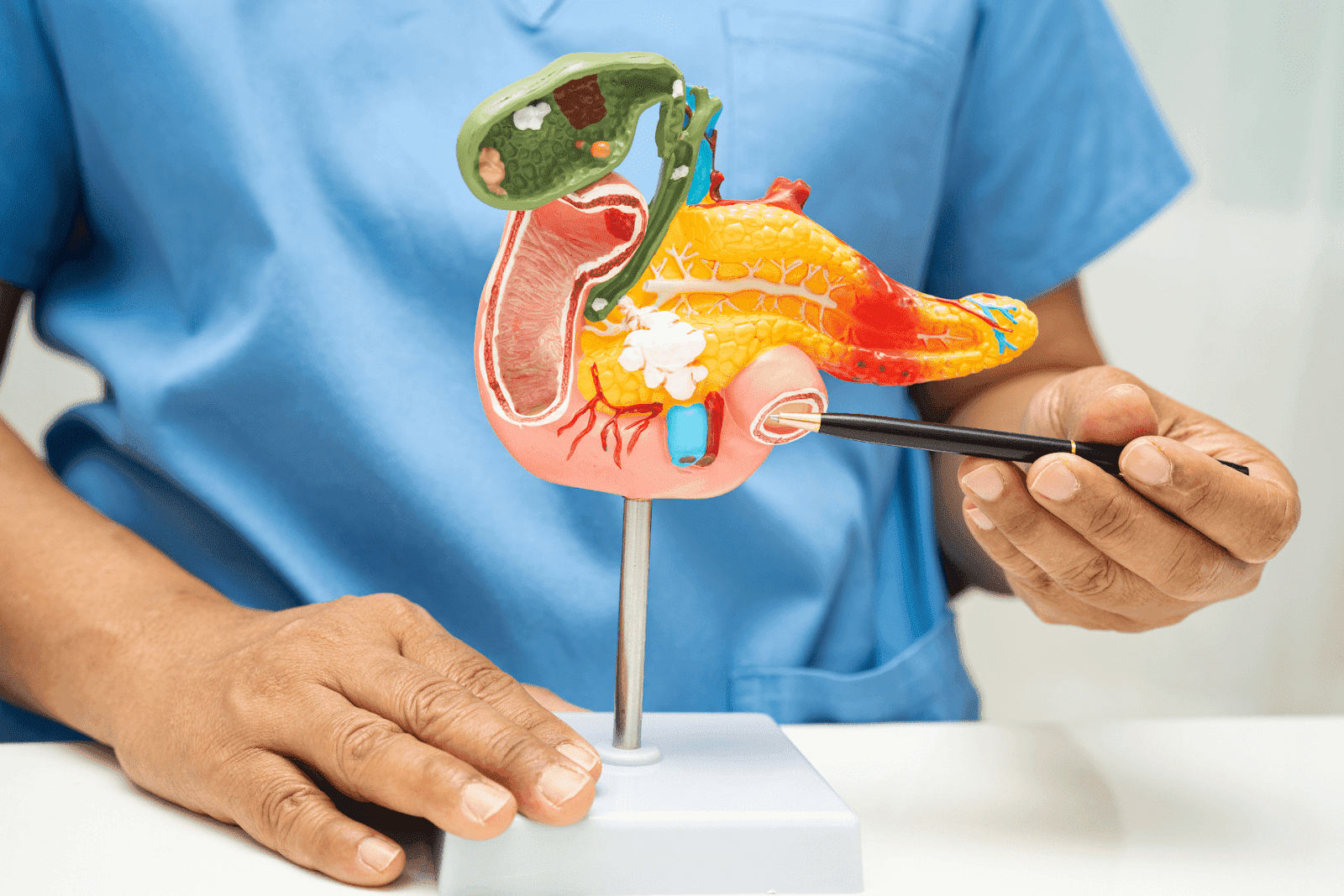
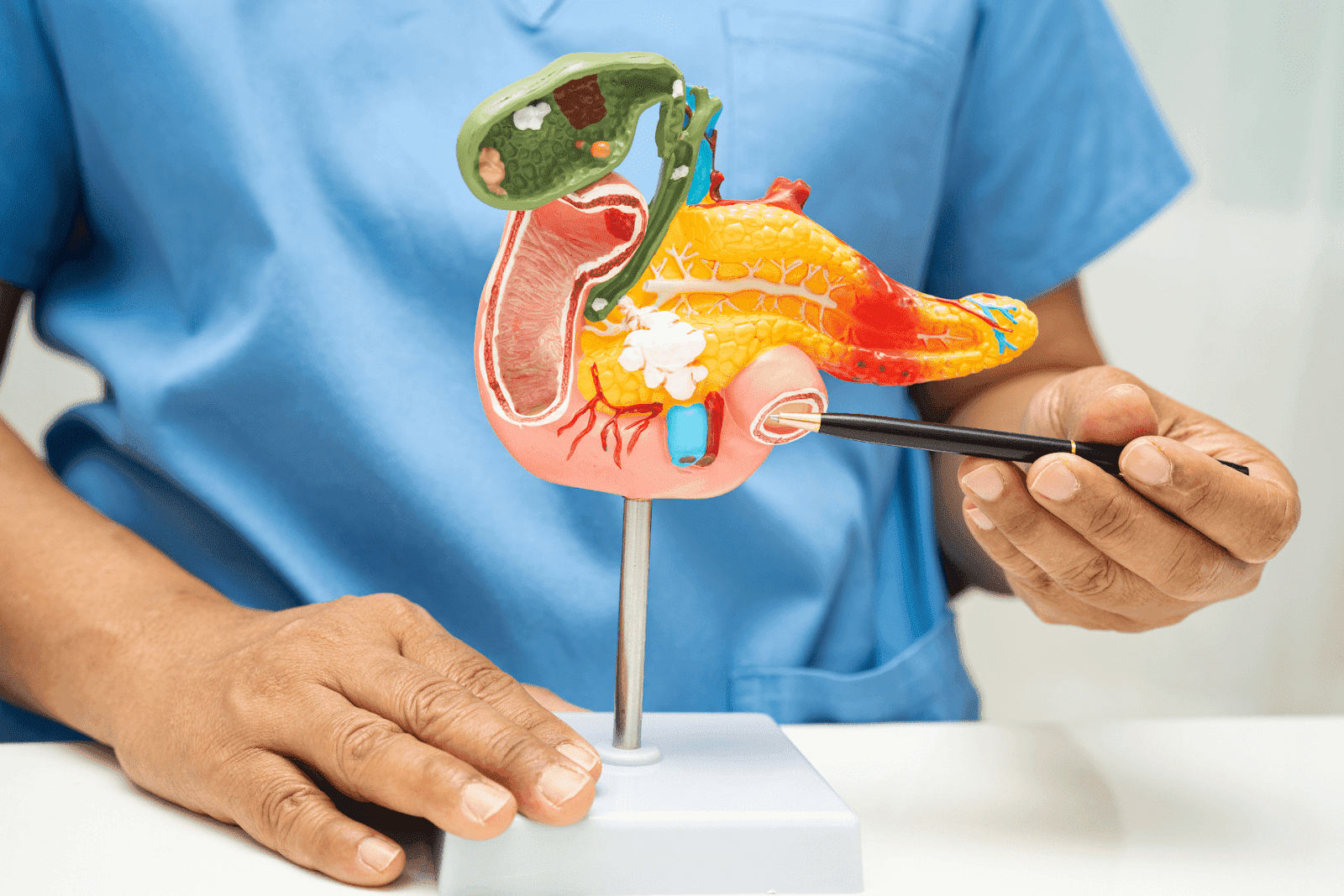
EPI is a condition where the pancreas fails to produce enough digestive enzymes necessary for breaking down food properly. These enzymes (lipase, protease, and amylase) are crucial for digesting fats, proteins, and carbohydrates. Without sufficient enzyme production, your body cannot absorb nutrients effectively, leading to malnutrition and a host of uncomfortable symptoms. Common symptoms of EPI include chronic diarrhea, weight loss, and abdominal pain, which can severely impact daily life and overall well-being.
The pancreas plays a vital role not only in digestion but also in regulating blood sugar through insulin production. However, EPI specifically refers to the malfunction of the exocrine part of the pancreas responsible for enzyme secretion. This condition can result from chronic pancreatitis, cystic fibrosis, pancreatic cancer, or other pancreatic disorders. In some cases, EPI can develop after surgical procedures that remove part of the pancreas or affect its function, further complicating the clinical picture.
 Why Is EPI Often Missed?
Why Is EPI Often Missed?
One of the challenges with EPI is that its symptoms overlap with many other digestive disorders, such as irritable bowel syndrome (IBS), lactose intolerance, or general indigestion. Patients may experience symptoms for months or even years without a proper diagnosis. Moreover, many healthcare providers may not immediately consider EPI, especially if the patient does not have a known history of pancreatic disease. This diagnostic delay can lead to a cycle of ineffective treatments and frustration for patients seeking relief.
Early diagnosis is critical because untreated EPI can lead to severe nutrient deficiencies, weight loss, and decreased quality of life. If you have ongoing digestive issues that don’t improve with standard treatments, it’s worth exploring whether EPI might be the cause. Diagnostic tests, such as stool tests that measure fat content or blood tests that assess enzyme levels, can help confirm the presence of EPI. Additionally, a thorough medical history and physical examination are essential to rule out other potential causes of the symptoms, ensuring that patients receive the appropriate care and management for their condition.
Recognizing the Symptoms of EPI
Identifying EPI can be tricky, but there are several hallmark symptoms to watch for. These symptoms result from poor digestion and nutrient absorption and can vary in severity depending on how advanced the condition is. The pancreas, which plays a crucial role in producing digestive enzymes, is often unable to meet the body's needs, leading to a cascade of digestive issues that can significantly impact quality of life.
Common Symptoms Include:
Chronic Diarrhea or Frequent Loose Stools: Due to undigested fats passing through the digestive tract, stools may be loose, greasy, or foul-smelling.
Steatorrhea: This refers to fatty stools that float and are difficult to flush, a classic sign of fat malabsorption.
Bloating and Gas: Undigested food ferments in the intestines, causing uncomfortable bloating and excessive gas.
Unexplained Weight Loss: Despite eating normally, nutrient malabsorption can lead to weight loss over time.
Fatigue and Weakness: Poor nutrient absorption can cause low energy levels and muscle weakness.
Abdominal Pain or Discomfort: Some patients report persistent abdominal pain or cramping.
It’s important to note that symptoms can be subtle in the early stages and may worsen gradually. If you notice a combination of these symptoms persisting for weeks or months, it’s advisable to seek medical evaluation. Early diagnosis is crucial, as untreated EPI can lead to serious complications, including vitamin deficiencies and osteoporosis. Furthermore, individuals may experience emotional and psychological effects due to the chronic nature of the condition, such as anxiety about eating or social situations where symptoms may become more pronounced.
In addition to these common symptoms, some individuals may also experience changes in appetite or food aversions, which can further complicate their nutritional intake. The interplay between EPI and other gastrointestinal disorders, such as irritable bowel syndrome (IBS) or celiac disease, can also obscure the diagnosis, making it essential for healthcare providers to conduct thorough evaluations. Diagnostic tests, including stool tests and imaging studies, can help confirm the presence of EPI and guide appropriate treatment options, which may include enzyme replacement therapy and dietary modifications to improve nutrient absorption.
How Is EPI Diagnosed?
Diagnosing EPI involves a combination of clinical evaluation, laboratory testing, and sometimes imaging studies. Because the symptoms overlap with other conditions, a thorough assessment is necessary to pinpoint the cause.
Tests Commonly Used to Diagnose EPI
Fecal Elastase Test: This is the most common non-invasive test for EPI. It measures the level of elastase, an enzyme produced by the pancreas, in stool samples. Low levels indicate pancreatic insufficiency.
72-Hour Fecal Fat Test: This test measures fat content in stool over three days to detect fat malabsorption.
Blood Tests: These can check for nutrient deficiencies such as low vitamin levels, anemia, or electrolyte imbalances.
Imaging Studies: Ultrasound, CT scans, or MRI may be used to evaluate the pancreas for structural abnormalities.
Because EPI can be linked to other pancreatic diseases, your healthcare provider may also investigate underlying causes to tailor treatment appropriately.
In addition to these tests, a detailed medical history and symptom diary can be invaluable for healthcare providers. Patients are often encouraged to note their dietary habits, frequency of gastrointestinal symptoms, and any other health issues that may be relevant. This comprehensive approach helps in understanding the full context of the patient's health and can reveal patterns that point toward EPI or other digestive disorders. Moreover, some patients may undergo genetic testing if there is a suspicion of hereditary conditions affecting pancreatic function, such as cystic fibrosis or hereditary pancreatitis.
Furthermore, the diagnostic process may also involve a trial of pancreatic enzyme replacement therapy (PERT) to see if symptoms improve. This can serve as both a diagnostic and therapeutic measure, as a positive response to treatment can confirm EPI. The healthcare provider may also recommend dietary modifications during this period to help manage symptoms and assess the effectiveness of the enzyme therapy. This multifaceted approach not only aids in accurate diagnosis but also helps in establishing a personalized treatment plan that addresses the unique needs of each patient.
Effective Treatment Options for EPI
The good news is that EPI is treatable, and with the right management, many patients experience significant symptom relief and improved quality of life.
Pancreatic Enzyme Replacement Therapy (PERT)
The cornerstone of EPI treatment is pancreatic enzyme replacement therapy. PERT involves taking prescription enzyme capsules with meals to aid digestion. These enzymes help break down fats, proteins, and carbohydrates, allowing your body to absorb nutrients effectively.
It’s essential to work closely with your healthcare provider to determine the correct dosage and timing of enzyme supplements. Adjustments may be needed based on your symptoms and dietary habits.
Dietary Modifications
Alongside enzyme therapy, dietary changes can help manage symptoms. Patients with EPI are often advised to:
Eat smaller, more frequent meals to ease digestive workload.
Limit high-fat foods if they exacerbate symptoms, but do not eliminate fats entirely without medical advice.
Ensure adequate intake of fat-soluble vitamins (A, D, E, K), which may require supplementation.
Consulting with a nutritionist experienced in digestive disorders can provide personalized guidance.
Why Telehealth Is a Game-Changer for Digestive Health Concerns
Accessing timely medical advice for digestive issues can sometimes be challenging, especially if symptoms are vague or intermittent. This is where telehealth services like Doctronic.ai come into play, revolutionizing how patients receive care.
Doctronic.ai offers AI-powered doctor visits that provide fast, personalized, and evidence-based medical guidance directly through their website. With over 10 million users and growing rapidly, Doctronic combines the latest peer-reviewed medical research with AI technology to deliver comprehensive answers and treatment recommendations in seconds.
Benefits of Using Doctronic.ai for Digestive Concerns
Speed: Get immediate answers to your health questions without waiting days for an appointment.
Expertise: The AI synthesizes the most current medical knowledge, ensuring you receive the best possible advice.
Personalized Care: The AI remembers your medical history and tailors recommendations to your unique situation.
Convenience: Access telehealth video visits with licensed doctors 24/7 for under $40, available in all 50 states.
If you suspect you might have EPI or are struggling with unexplained digestive symptoms, starting with a free AI doctor visit at Doctronic.ai can be an excellent first step. You can receive a preliminary assessment and guidance on next steps, including whether to pursue further testing or specialist referral.
 When to See a Doctor in Person
When to See a Doctor in Person
While telehealth can provide rapid initial evaluation, certain situations require in-person medical attention. If you experience severe abdominal pain, persistent vomiting, unexplained weight loss, or signs of malnutrition, it is important to consult a healthcare provider promptly.
For ongoing management of EPI, your doctor may coordinate care involving gastroenterologists, dietitians, and other specialists. Regular follow-up is essential to monitor treatment effectiveness and adjust therapy as needed.
Living Well With EPI: Tips and Considerations
Managing EPI is a lifelong commitment, but with the right approach, individuals can lead healthy, active lives. Here are some practical tips for living well with EPI:
Stay Consistent with Enzyme Therapy: Take your enzymes exactly as prescribed with every meal and snack.
Monitor Symptoms: Keep a symptom diary to track what foods or activities trigger discomfort.
Maintain Regular Medical Care: Schedule routine check-ups to assess nutritional status and pancreatic function.
Stay Informed: Advances in pancreatic health and digestive care continue to evolve. Using Doctronic.ai can keep you updated on the latest recommendations.
Seek Support: Connect with patient groups or counseling services if coping with a chronic condition feels overwhelming.
Fast Answers for Digestive Concerns
Digestive difficulties can be frustrating and debilitating, but they don’t have to be endured in silence or confusion. Exocrine Pancreatic Insufficiency is a treatable condition that may be the root cause of your symptoms. Recognizing the signs, seeking timely diagnosis, and initiating proper treatment can dramatically improve your quality of life.
Thanks to innovations in healthcare technology, Doctronic.ai makes it easier than ever to access expert medical advice from the comfort of your home. Whether you want a quick AI-powered consultation or a telehealth video visit with a licensed doctor, Doctronic offers a smart, fast, and affordable way to address your digestive health concerns.
Take Control of Your Digestive Health with Doctronic
If you're tired of struggling with digestive issues and suspect EPI might be the culprit, Doctronic is here to help. Experience the most modern, personal, and intelligent healthcare solution available. Our AI-powered doctor is ready to provide you with a free, comprehensive assessment based on the latest medical research, all within seconds. Say goodbye to waiting rooms and enjoy the convenience of 24/7 access to our telehealth services in all 50 states. Skip the line. Talk to an AI Doctor Now, for free.



 Why Is EPI Often Missed?
Why Is EPI Often Missed? When to See a Doctor in Person
When to See a Doctor in Person