Pain at the base of the skull can be perplexing and uncomfortable. It can stem from various causes, ranging from tension headaches to more serious medical conditions.
Understanding the potential reasons behind this discomfort is crucial for effective management and treatment. This article delves into the various causes, symptoms, and treatment options for pain at the base of the skull.
Understanding the Anatomy
Understanding the anatomy of the base of the skull is essential to comprehending the reasons behind pain at this location. The base of the skull is home to several critical structures, including muscles, nerves, and blood vessels.
This region serves as a vital junction between the brain and the spinal cord, playing a crucial role in the overall functionality of the nervous system.
 The Musculoskeletal Structure
The Musculoskeletal Structure
The muscles at the base of the skull play a significant role in supporting the head and facilitating movement. Tightness or strain in these muscles can lead to discomfort. Key muscles include:
Trapezius
Splenius capitis
Suboccipital muscles
Additionally, the intricate arrangement of these muscles allows for a wide range of head movements, from nodding to rotation.
The trapezius, for example, extends down the back and helps in shrugging the shoulders, while the splenius capitis assists in extending and rotating the head.
When these muscles become tense due to poor posture, stress, or overuse, they can contribute significantly to pain and discomfort at the base of the skull.
Nerve Pathways
The cervical spine houses several nerves that can contribute to pain when irritated or compressed. The greater occipital nerve is particularly noteworthy, as it can cause pain that radiates from the base of the skull to the scalp.
This nerve, along with others like the lesser occipital nerve, can become entrapped or inflamed, leading to conditions such as occipital neuralgia, which is characterized by sharp, shooting pain.
Moreover, the interplay between these nerves and the surrounding muscles is complex. For instance, muscle tension can lead to nerve compression, which in turn can exacerbate muscle tightness, creating a vicious cycle of pain.
Understanding this relationship is crucial for effective treatment and management of pain in this area, as targeted therapies may help alleviate both muscular and nerve-related discomfort.
Common Causes of Pain at the Base of the Skull
Identifying the underlying cause of pain at the base of the skull is vital for effective treatment. Here are some common causes:
Tension Headaches
Tension headaches are one of the most prevalent causes of pain at the base of the skull. They often arise from muscle tension and stress, leading to discomfort that can feel like a tight band around the head. These headaches can be triggered by a variety of factors, including poor posture, prolonged screen time, and emotional stress.
Symptoms: Dull, aching pain, tightness in the neck and shoulders, and sensitivity to light.
Management: Over-the-counter pain relievers, relaxation techniques, and physical therapy.
Cervicogenic Headaches
Cervicogenic headaches originate from the cervical spine and can manifest as pain at the base of the skull.
They often occur due to neck injuries or degenerative conditions. The pain may be exacerbated by certain neck movements or positions, making it crucial to identify and address the underlying neck issues.
Symptoms: Pain on one side of the head, neck stiffness, and reduced range of motion.
Management: Physical therapy, chiropractic adjustments, and medications.
Occipital Neuralgia
Occipital neuralgia is characterized by irritation or injury to the occipital nerves, resulting in sharp, shooting pain at the base of the skull. This condition can be triggered by various factors, including trauma or inflammation.
Patients may also experience episodes of pain that can be triggered by simple actions such as turning the head or even brushing the hair.
Symptoms: Intense, electric shock-like pain, tenderness at the base of the skull, and sensitivity to touch.
Management: Nerve blocks, physical therapy, and medications to alleviate nerve pain.
Muscle Strain
Muscle strain in the neck can also contribute to pain at the base of the skull. This strain can result from overexertion during physical activities, sleeping in an awkward position, or even stress that leads to muscle tightness.
The discomfort may radiate to the shoulders and upper back, compounding the sensation of pain and discomfort.
Symptoms: Localized pain in the neck, stiffness, and muscle spasms.
Management: Rest, ice or heat application, and gentle stretching exercises.
Arthritis
Arthritis, particularly osteoarthritis, can also affect the cervical spine and lead to pain at the base of the skull.
As the cartilage in the joints wears down, it can cause inflammation and pain, which may be felt not only in the neck but also radiating towards the head. This condition is more common in older adults but can also occur in younger individuals due to previous injuries or genetic factors.
Symptoms: Chronic pain, stiffness, and swelling in the neck area.
Management: Anti-inflammatory medications, physical therapy, and in severe cases, surgical intervention.
Less Common Causes
While the aforementioned causes are common, several less frequent conditions can also lead to pain at the base of the skull. Understanding these can help in recognizing when to seek medical attention.
Arthritis
Arthritis in the cervical spine can lead to inflammation and pain at the base of the skull. Osteoarthritis and rheumatoid arthritis are two types that may affect this area. The degeneration of cartilage in osteoarthritis can result in bone spurs, which may further irritate surrounding tissues and nerves, leading to discomfort.
In contrast, rheumatoid arthritis is an autoimmune disorder that can cause chronic inflammation, potentially affecting multiple joints and leading to systemic symptoms.
Symptoms: Stiffness, swelling, and pain that worsens with movement.
Management: Anti-inflammatory medications, physical therapy, and in severe cases, surgical intervention.
Infections
Infections such as meningitis can cause severe pain at the base of the skull, often accompanied by other systemic symptoms. Meningitis, an inflammation of the protective membranes covering the brain and spinal cord, can be caused by viral, bacterial, or fungal infections.
The rapid onset of symptoms and the potential for serious complications make prompt medical attention crucial in these cases. Other infections, such as osteomyelitis of the cervical vertebrae, can also lead to localized pain and require immediate evaluation.
Symptoms: Fever, neck stiffness, and sensitivity to light.
Management: Hospitalization and antibiotic treatment.
Fibromyalgia
Fibromyalgia is a chronic condition characterized by widespread pain, including at the base of the skull. It often coexists with other symptoms such as fatigue and sleep disturbances.
The exact cause of fibromyalgia is still not fully understood, but it is believed to involve abnormal pain processing in the brain and spinal cord.
Patients may also experience heightened sensitivity to pain, known as allodynia, where even light touch can be painful. This condition can significantly impact daily life, making it essential for individuals to seek a comprehensive management plan.
Symptoms: Chronic pain, tenderness, and cognitive difficulties.
Management: Medications, lifestyle changes, and cognitive-behavioral therapy.
 Symptoms to Watch For
Symptoms to Watch For
While pain at the base of the skull can often be attributed to benign causes, certain symptoms warrant immediate medical attention.
Recognizing these symptoms can be crucial for timely intervention. It's important to be aware of the nuances of pain and accompanying signs, as they can provide insight into the underlying issue.
For instance, tension headaches may produce discomfort in this area, but they typically lack the severity and additional symptoms associated with more serious conditions.
Red Flags
Some symptoms that may indicate a more serious underlying condition include:
Severe, sudden onset of pain
Pain accompanied by fever or chills
Neurological symptoms such as weakness, numbness, or vision changes
In addition to these red flags, other concerning signs may include persistent vomiting, difficulty swallowing, or changes in mental status, such as confusion or difficulty concentrating.
These symptoms can suggest more complex issues, such as infections or inflammatory conditions affecting the brain or spinal cord.
It’s essential to take note of the context in which these symptoms arise; for example, if they follow a recent head injury or are linked to a history of migraines, this information can be vital for healthcare providers in determining the appropriate course of action.
When to Seek Medical Help
If pain at the base of the skull persists for an extended period or is accompanied by any of the red flag symptoms, it is advisable to consult a healthcare professional. Early diagnosis can lead to more effective treatment.
Furthermore, keeping a detailed record of the pain's characteristics—such as its intensity, duration, and any triggers—can aid your healthcare provider in making a more accurate diagnosis.
This proactive approach not only helps in identifying the root cause but also empowers patients to engage actively in their health management, leading to better outcomes.
Diagnosis of Pain at the Base of the Skull
Diagnosing the cause of pain at the base of the skull typically involves a thorough medical history and physical examination. Healthcare providers may also utilize various diagnostic tools to pinpoint the underlying issue.
Understanding the specific characteristics of the pain, such as its intensity, quality, and any associated symptoms, can significantly aid in the diagnostic process.
Medical History and Physical Examination
The healthcare provider will ask about the patient's symptoms, duration, and any potential triggers. A physical examination may include:
Additionally, the provider may inquire about the patient's lifestyle, including any recent injuries, stress levels, and overall physical activity. These factors can provide crucial insights into the potential causes of pain.
For instance, a history of poor posture or prolonged computer use may suggest tension headaches or muscle strain as contributing factors.
Furthermore, understanding the patient's medical history, including any previous neck injuries or chronic conditions, can help in identifying patterns that may be relevant to the current symptoms.
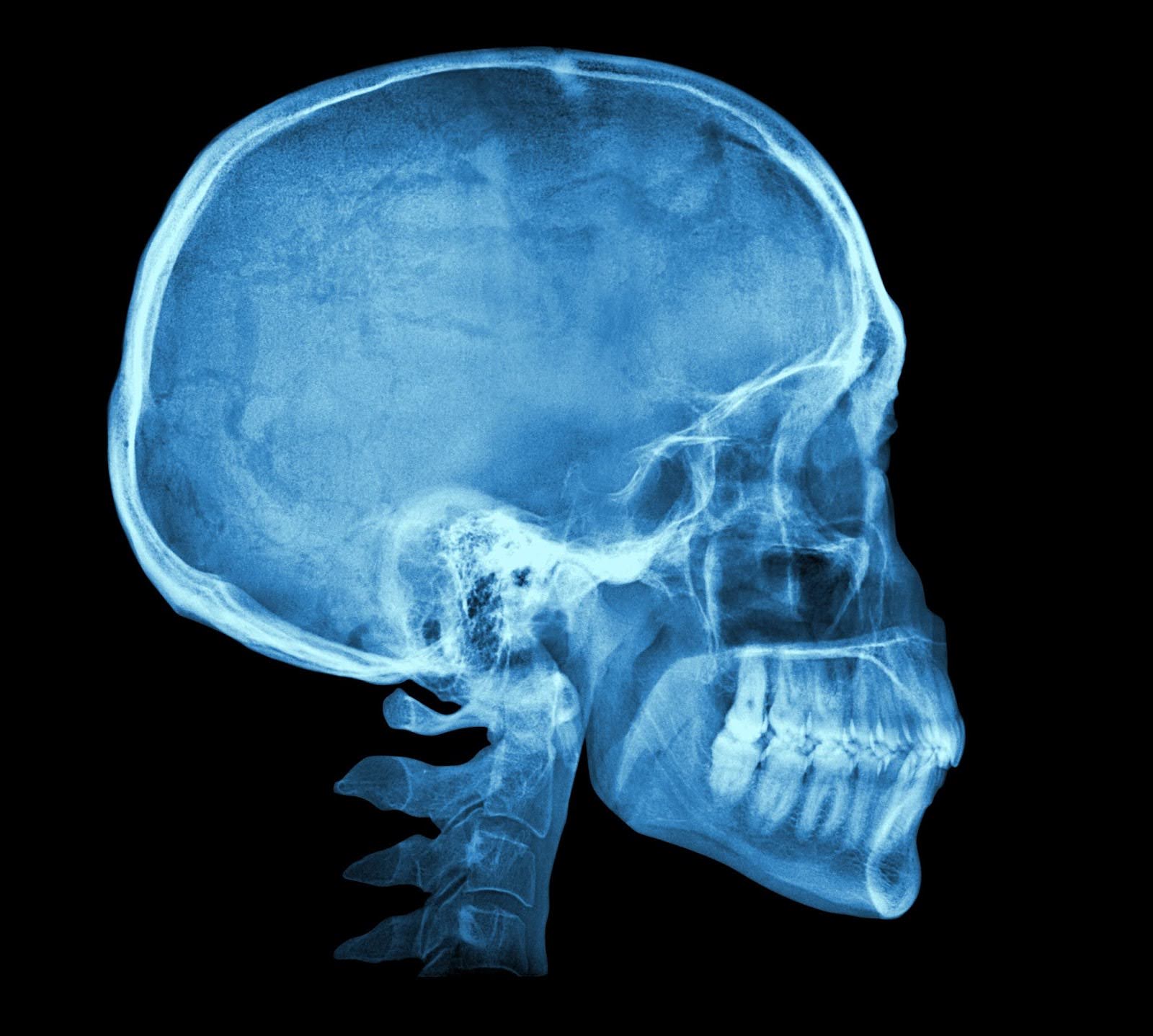
Imaging Studies
If the initial assessment suggests a more serious condition, imaging studies may be ordered. Common imaging techniques include:
X-rays: To check for structural abnormalities in the cervical spine.
MRIs: To visualize soft tissues, including nerves and muscles.
CT scans: To provide detailed images of the bones and joints.
In some cases, additional specialized imaging, such as a functional MRI or a myelogram, may be recommended to further investigate the cause of pain.
These advanced imaging techniques can help detect subtle changes in the spinal cord or nerve roots that may not be visible on standard X-rays or MRIs.
Moreover, the interpretation of these images often requires collaboration between radiologists and specialists, ensuring a comprehensive understanding of the patient's condition and guiding appropriate treatment options.
Treatment Options
Treatment for pain at the base of the skull varies depending on the underlying cause. A combination of therapies may be employed to alleviate symptoms and address the root issue.
Medications
Medications can play a significant role in managing pain at the base of the skull. Depending on the diagnosis, the following types of medications may be used:
Over-the-counter pain relievers: Such as ibuprofen or acetaminophen for mild to moderate pain.
Prescription medications: Muscle relaxants or stronger pain relievers for more severe discomfort.
Antidepressants: May be prescribed for conditions like fibromyalgia.
Physical Therapy
Physical therapy can be beneficial in addressing musculoskeletal issues. A physical therapist may develop a personalized program that includes:
Alternative Therapies
In addition to traditional treatments, alternative therapies may provide relief for some individuals. These can include:
Chiropractic care: To realign the spine and relieve pressure on nerves.
Acupuncture: To promote pain relief through targeted stimulation of specific points.
Massage therapy: To alleviate muscle tension and improve circulation.
Preventive Measures
Preventing pain at the base of the skull often involves lifestyle adjustments and ergonomic considerations. Here are some strategies to consider:
Ergonomics
Maintaining proper posture while sitting, especially during long hours at a desk, can significantly reduce strain on the neck and shoulders. Consider the following:
Adjust the height of your chair and desk to keep your computer screen at eye level.
Use a chair that provides adequate lumbar support.
Take regular breaks to stretch and move around.
Stress Management
Stress can contribute to muscle tension, leading to pain at the base of the skull. Incorporating stress management techniques can be beneficial:
Practicing mindfulness or meditation.
Engaging in regular physical activity.
Ensuring adequate sleep and relaxation.
Regular Exercise
Regular exercise can strengthen the muscles supporting the neck and improve overall flexibility. Activities such as yoga, pilates, and swimming can be particularly beneficial in maintaining a healthy musculoskeletal system.
Understand and Manage Neck Pain Better with Doctronic’s AI Support
Pain at the base of the skull can stem from many causes, ranging from simple tension headaches to more complex medical conditions. As explored in this article, identifying the root cause is crucial for effective treatment and long-term relief.
By paying attention to symptoms, seeking timely medical guidance, and adopting preventive habits, individuals can take meaningful steps toward managing discomfort and improving their daily lives.
That’s where Doctronic comes in. As the #1 AI Doctor, Doctronic offers free AI doctor visits to help users better understand their symptoms from the comfort of home. Whether it’s neck pain or another health concern, our AI delivers fast, reliable insights that you can use when speaking with a healthcare provider.


 The Musculoskeletal Structure
The Musculoskeletal Structure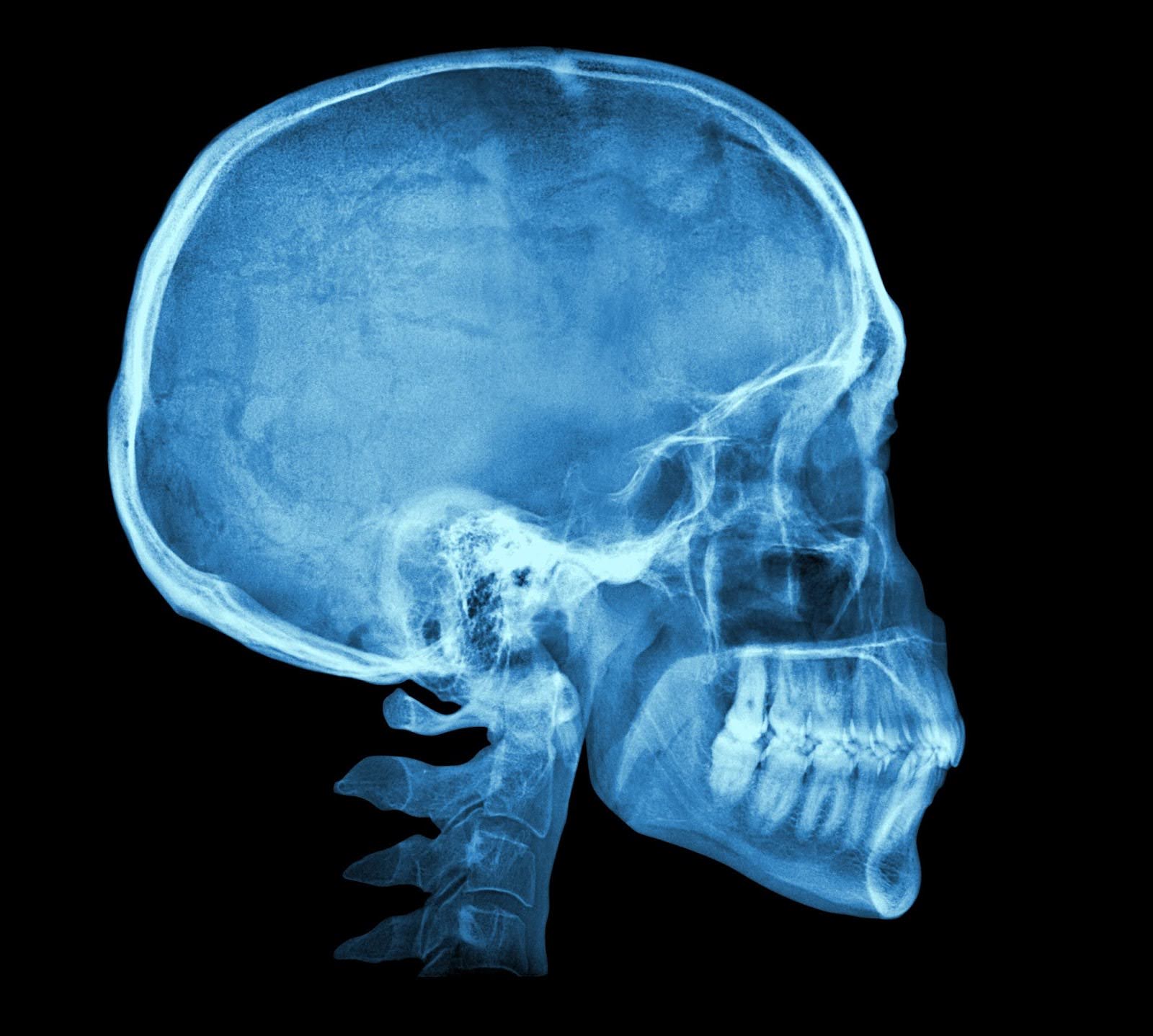 Symptoms to Watch For
Symptoms to Watch For