Standing Desks for Back Pain: Pros and Cons
The Relationship Between Sedentary Work and Spinal HealthYour spine was not designed for eight hours of sitting. The human body evolved for movement, yet modern office work [...]
Read More
Medically reviewed by Alan Lucks | MD, Alan Lucks MDPC Private Practice - New York on October 10th, 2025.
This condition affects women 7 times more frequently than men and impacts 2-4% of the population, with widespread musculoskeletal pain persisting for at least 3 months as the primary diagnostic criterion.
Beyond pain, patients experience "fibro fog" (cognitive difficulties with memory and concentration), heightened sensitivity to touch, light, and sound, plus chronic sleep disruption that worsens other symptoms.
Physical trauma, viral infections, and severe emotional stress can trigger onset in genetically predisposed individuals, with family history being a significant risk factor.
First-line medications include duloxetine (an antidepressant) and pregabalin (an anticonvulsant), which target nerve pain pathways rather than traditional pain relievers like NSAIDs or opioids.
Proper diagnosis requires excluding thyroid disorders, vitamin D deficiency, and autoimmune conditions through blood work, since these conditions can mimic the widespread pain and fatigue patterns.
Chronic, widespread pain can be confusing and isolating. When the usual tests come back normal, and pain persists for months or years, fibromyalgia is often the diagnosis that explains a complex pattern of symptoms. Recognizing fibromyalgia early can open the door to effective symptom management, better sleep, and improved quality of life. This article explains what fibromyalgia looks like, how it’s diagnosed, common mimics, and practical steps to get the right care, including how AI-powered telehealth like Doctronic.ai can help guide next steps.
Fibromyalgia is a chronic pain condition characterized by widespread musculoskeletal pain accompanied by fatigue, sleep disturbances, cognitive symptoms, and mood changes. It is a disorder of pain processing in the central nervous system: the brain and spinal cord amplify pain signals, creating a heightened sensitivity to pressure, touch, and sometimes normal sensations.
Prevalence estimates vary, but fibromyalgia affects roughly 2% to 4% of the general population, with higher rates in women. Symptoms often start in middle adulthood but can appear at any age. Many people with fibromyalgia also have other conditions such as irritable bowel syndrome (IBS), migraines, temporomandibular joint disorder (TMJ), and mood or anxiety disorders.
 Key Symptoms to Watch For
Key Symptoms to Watch ForFibromyalgia does not cause visible inflammation or structural damage that appears on routine imaging. Instead, it is diagnosed based on symptom patterns and the exclusion of other conditions. Recognizing the characteristic cluster of symptoms is the first step.
Pain is the hallmark. It tends to be diffuse, affecting both sides of the body and both above and below the waist. People often describe it as aching, burning, or stabbing, and it may shift locations from day to day. Unlike pain from a single injured tendon or joint, fibromyalgia pain is generalized.
Waking unrefreshed despite adequate time in bed is common. Sleep may be fragmented, and non-restorative sleep contributes to daytime fatigue and cognitive fog. Many people with fibromyalgia report waking frequently and still feeling exhausted.
Problems with attention, memory, processing speed, or finding words, often called “fibro fog”, are frequent and can interfere with work and daily tasks. Mental fatigue is as disabling as physical fatigue for many people.
Increased sensitivity to pressure, light, noise, smells, or temperature changes is common. Some people experience numbness, tingling, or a burning sensation without clear nerve injury.
Many people also report headaches or migraines, IBS-like digestive symptoms, pelvic pain, restless legs, and mood symptoms such as anxiety or depression. These overlapping conditions can complicate diagnosis and management.
There is no single blood test or scan that proves fibromyalgia. Diagnosis relies on a careful clinical history, symptom assessment, and ruling out other possible causes. Diagnostic criteria developed by rheumatology associations have moved away from tender-point exams toward standardized symptom scoring.
Modern diagnostic approaches use tools like the Widespread Pain Index and Symptom Severity scores that quantify how many body regions are painful and how severe symptoms such as fatigue, unrefreshing sleep, and cognitive symptoms are. These scales help standardize the diagnosis and monitor changes over time.
Because many medical and rheumatologic conditions can cause widespread pain, clinicians often order blood tests to exclude inflammatory arthritis, thyroid dysfunction, vitamin D deficiency, or other metabolic problems. Basic labs might include a complete blood count (CBC), metabolic panel, thyroid-stimulating hormone (TSH), and sometimes markers of inflammation such as ESR or CRP. Normal results on these tests, combined with characteristic symptom patterns, support a fibromyalgia diagnosis.
Imaging, like X-rays or MRI, is used selectively to evaluate localized pain or rule out structural causes, but imaging alone won’t confirm fibromyalgia.
Understanding overlapping conditions helps prevent misdiagnosis and ensures targeted treatment. Fibromyalgia often coexists with other disorders, and treating those conditions can improve overall symptoms.
Conditions such as rheumatoid arthritis, systemic lupus erythematosus, and polymyalgia rheumatica can present with pain and fatigue. These illnesses usually show objective signs, joint swelling, elevated inflammatory markers, or specific autoantibodies, so appropriate testing helps differentiate them from fibromyalgia.
Thyroid disorders (hypothyroidism), vitamin D deficiency, and other metabolic problems can cause fatigue and muscle aches. Simple blood tests can detect these treatable conditions.
Nerve compression, diabetic neuropathy, or small-fiber neuropathy may produce burning, tingling, or numbness. Neurological examination and specific tests, including nerve conduction studies or referrals to neurology, can help distinguish these causes.
Certain infections may trigger prolonged symptoms. A careful history, recent infections, Lyme disease risk, or persistent viral symptoms can guide testing when clinically appropriate.
Fibromyalgia treatment focuses on symptom management and improving function, rather than curing the condition. A combination of medication, exercise, sleep optimization, psychological therapies, and lifestyle adjustments usually works best. Personalized plans tailored to symptom severity and patient preferences provide the most benefit.
Several medications have evidence for reducing pain and improving sleep in fibromyalgia. These include certain antidepressants (such as SNRIs and tricyclics), anti inflammatory medicines, anticonvulsants (gabapentin, pregabalin), and medications targeting sleep. Opioids are generally not recommended because they are often ineffective for central pain processes and carry a high risk.
Medication choice depends on coexisting conditions, side effect profiles, and goals. Working with a clinician to start low and go slow with doses helps minimize side effects.
Regular, graded exercise is one of the most effective non-drug treatments. Low-impact aerobic activities (walking, swimming, cycling), gentle strength training, and stretching programs reduce pain and improve function. Starting slowly and increasing activity gradually prevents flare-ups and builds confidence.
Cognitive behavioral therapy (CBT), pain coping skills, and graded exposure therapies help reframe pain responses and reduce disability. Psychological therapies also address comorbid anxiety or depression and improve sleep hygiene and daily routines.
Improving sleep quality is critical. Strategies include consistent sleep schedules, limiting caffeine and electronics before bed, and treating restless legs or sleep apnea if present. Addressing sleep often reduces pain and fatigue significantly.
Pacing activity, setting realistic goals, and using energy-conservation techniques help prevent cycles of overactivity and flare-ups. Tracking symptom triggers, such as poor sleep, stress, or weather changes, helps identify actionable adjustments.
Persistent widespread pain, ongoing fatigue, and cognitive difficulties that interfere with daily life merit a medical evaluation. Primary care clinicians and specialists (rheumatology, neurology, pain medicine) will take a comprehensive history and tailor testing to rule out other diagnoses.
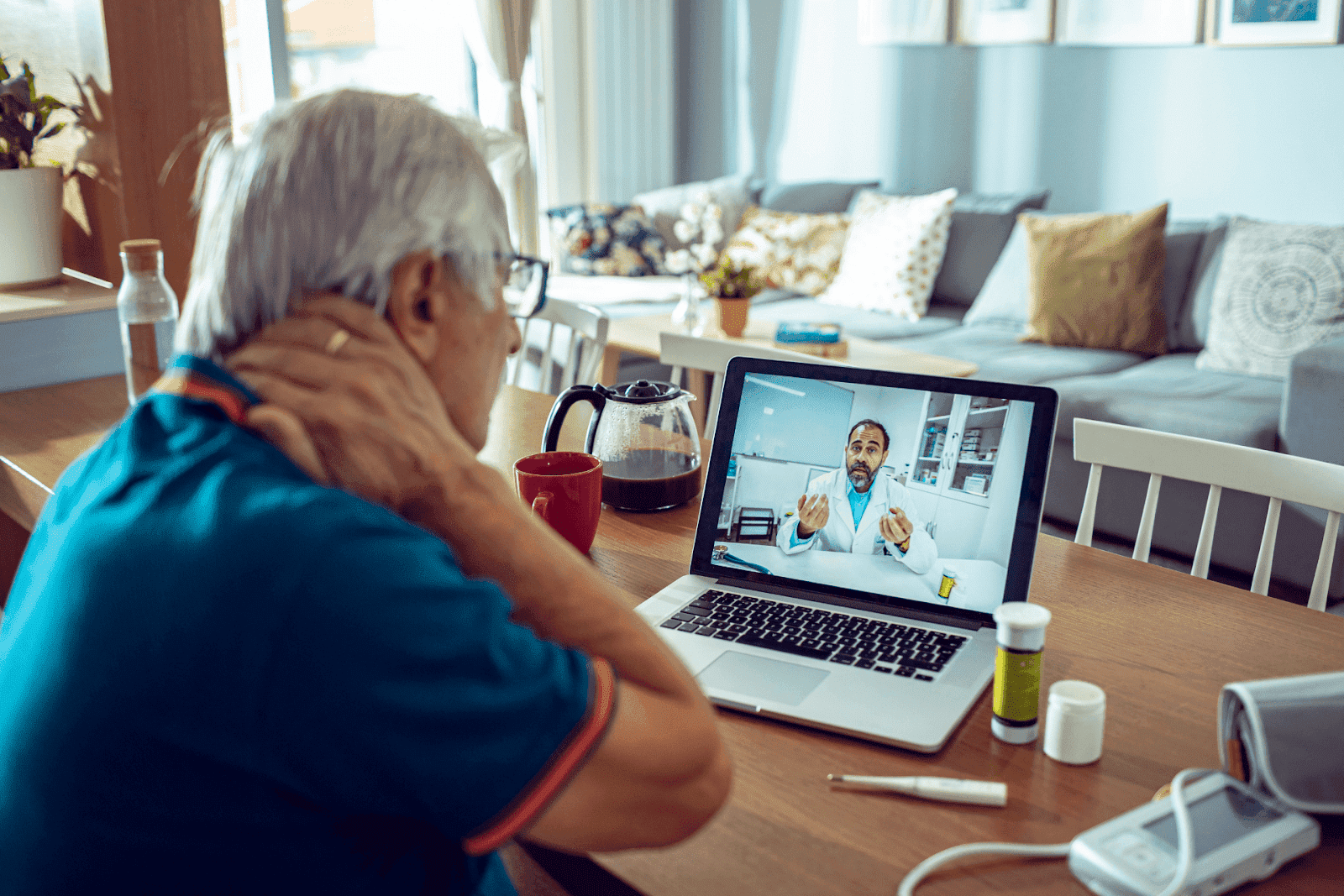
Accessing care quickly is essential for minimizing disability. AI-powered services now offer immediate, evidence-informed guidance and convenient follow-up options. Doctronic.ai provides free AI doctor visits through its website that synthesizes the latest peer-reviewed medical literature to give a thorough initial assessment. These AI visits can produce clear, shareable summaries to take to a clinician for confirmatory testing or in-person care.
For those who want a live clinical visit, Doctronic also offers affordable telehealth video visits with licensed doctors 24/7 across all 50 states for under $40. This combination, a rapid AI-based assessment followed by an inexpensive telehealth visit when needed, can speed diagnosis, coordinate tests, and begin a treatment plan without long wait times or expensive clinic visits. Visit Doctronic.ai to try the AI doctor or schedule a telehealth video visit.
Most fibromyalgia-related symptoms are chronic and non-emergent. However, certain red flags require prompt medical evaluation to exclude serious conditions. Seek urgent care or emergency services if new, severe symptoms occur.
Sensory loss, progressive weakness, sudden severe localized pain, unexplained fever, or rapidly worsening neurological symptoms (loss of bowel or bladder control, severe numbness) are not typical features of fibromyalgia and warrant immediate assessment. If infection, cancer, or acute neurological disease is suspected, speedy evaluation is essential.
When seeking immediate in-person care, it is important to rely on verified, up-to-date resources. Doctronic does not provide a directory of urgent care locations, hours, or patient reviews; use local health systems, emergency lines, or trusted regional resources to identify appropriate urgent care centers.
Small, consistent changes often lead to significant improvements in symptoms and quality of life. Building a toolkit of strategies tailored to lifestyle and preferences empowers long-term management.
Start with realistic, calming morning routines and prioritize consistent bedtimes. Light exposure in the morning, brief movement, and minimizing naps can help regulate sleep-wake cycles and reduce daytime fatigue.
Short, regular bouts of movement beat occasional intense exercise for preventing flare-ups. Gentle stretching, tai chi, or water-based exercises are especially helpful for people with high pain sensitivity.
Mindfulness, deep-breathing exercises, and structured relaxation practices lower stress hormones that can exacerbate pain. Social support and setting boundaries at work and home also protect energy reserves.
Maintaining balanced nutrition and adequate hydration supports overall health. While no single diet cures fibromyalgia, some people find symptom relief from identifying food sensitivities, reducing processed foods, and moderating caffeine and alcohol intake.
Fibromyalgia is a chronic condition for most people, and ongoing follow-up with clinicians helps adapt treatment plans as symptoms change. Interdisciplinary care, involving primary care, rheumatology, physical therapy, behavioral health, and community supports, provides the best outcomes.
Digital symptom trackers, telehealth follow-ups, and AI-powered check-ins can streamline care. Doctronic.ai’s platform enables quick AI assessments and accessible telehealth visits that can be used regularly to adjust medications, monitor progress, and coordinate referrals. This kind of continuity helps treatment stay aligned with changing needs without the friction of long waits or costly visits.
 Early Recognition Matters
Early Recognition MattersChronic widespread pain that interferes with daily life deserves evaluation. Recognizing the triad of widespread pain, sleep disturbance, and cognitive symptoms can point clinicians toward a fibromyalgia diagnosis and a comprehensive management plan. Early multimodal treatment, combining medication when appropriate, exercise, sleep optimization, psychological therapies, and pacing, produces the best long-term outcomes.
For those seeking a quick, evidence-informed first step, the AI doctor at Doctronic.ai provides free, literature-backed guidance and clear next steps. When an in-person or live telehealth visit is needed, Doctronic’s affordable 24/7 video visits connect patients with licensed clinicians across all 50 states for under $40, making ongoing care more accessible. Start with an assessment, gather a concise symptom summary, and work with a clinician to build a sustainable plan for living well with fibromyalgia. Visit Doctronic.ai to learn more and get started today.
Effective management focuses on symptom control through a combination of specific medications, low-impact exercise, and sleep optimization rather than pursuing a cure. Early diagnosis is crucial because proper treatment can significantly improve quality of life and prevent symptom progression. If you're experiencing persistent widespread pain with fatigue that's affecting your daily activities, Doctronic can help you get the proper evaluation and answers you need.
The Relationship Between Sedentary Work and Spinal HealthYour spine was not designed for eight hours of sitting. The human body evolved for movement, yet modern office work [...]
Read MoreLiving with Sciatica Means Knowing Your LimitsThat shooting pain down the leg affects more people than most realize. As many as 40% of Americans will experience sciatica at [...]
Read MoreWhat Tech Neck Is and Why It’s So CommonYour neck was not designed for smartphones. The human spine evolved over millions of years to support a head positioned directly above [...]
Read More