Lipedema and lymphedema are two distinct conditions that often get confused due to their similar names and overlapping symptoms. However, understanding the differences between them is crucial for effective management and treatment. This article aims to clarify the characteristics, causes, symptoms, and treatment options for both conditions, providing a comprehensive overview to help individuals differentiate between lipedema and lymphedema.
 Understanding Lipedema
Understanding Lipedema
What is Lipedema?
Lipedema is a chronic condition characterized by an abnormal accumulation of fat, primarily in the lower body, including the hips, thighs, and calves. This condition predominantly affects women and is often mistaken for general obesity or lymphedema. Unlike typical fat distribution, lipedema fat is resistant to diet and exercise, leading to disproportionate body shapes. The condition can lead to significant physical discomfort and emotional distress, as many women struggle with the societal pressures surrounding body image and weight. Understanding lipedema is crucial for both patients and healthcare providers, as it requires a tailored approach to treatment and management.
Causes of Lipedema
The exact cause of lipedema remains unclear, but it is believed to have a genetic component. Many women with lipedema have a family history of the condition, suggesting a hereditary link. Hormonal changes, particularly those related to puberty, pregnancy, and menopause, may also trigger or exacerbate lipedema symptoms. Research is ongoing to explore the role of hormones and other biological factors in the development of lipedema, and some studies suggest that inflammation may also play a role in the condition's progression. Understanding these underlying factors is essential for developing effective treatment strategies.
Symptoms of Lipedema
Symmetrical swelling in the legs and buttocks
Easy bruising
Discomfort or pain in the affected areas
Skin texture changes, such as a dimpled appearance
Increased sensitivity to touch
As the condition progresses, individuals may experience mobility issues and psychological impacts due to changes in body image. Early recognition and intervention are essential for effective management. Patients often report feelings of frustration and isolation, as lipedema can be misunderstood by both the public and medical professionals. Support groups and educational resources can provide a sense of community and understanding, helping individuals navigate the complexities of living with lipedema.
Additionally, advancements in treatment options, including specialized therapies and surgical interventions, are being explored to improve the quality of life for those affected by this challenging condition.
Understanding Lymphedema
What is Lymphedema?
Lymphedema is a condition that results from a compromised lymphatic system, leading to the accumulation of lymphatic fluid in tissues. This condition can occur in any part of the body, but is most commonly observed in the arms and legs. Lymphedema can be classified as primary, which is often hereditary, or secondary, which can result from surgery, radiation, or trauma. The lymphatic system plays a crucial role in maintaining fluid balance and immune function, making lymphedema not just a cosmetic concern but a significant health issue that can affect overall well-being.
Causes of Lymphedema
Primary lymphedema is caused by developmental abnormalities in the lymphatic system, while secondary lymphedema is often a consequence of damage to the lymphatic vessels. Common causes include:
Cancer treatments, such as lymph node removal or radiation
Infections
Trauma or injury to the lymphatic system
Obesity, which can put additional pressure on the lymphatic vessels
Recognizing the underlying cause is vital for determining the most effective treatment approach. In addition to these factors, certain medical conditions, such as chronic venous insufficiency and filariasis, can also contribute to the development of lymphedema. Understanding these causes helps healthcare professionals tailor their interventions to address the specific needs of the patient, which can significantly improve quality of life.
Symptoms of Lymphedema
Symptoms of lymphedema can vary but typically include:
Swelling in the affected limb or area
A feeling of heaviness or tightness
Restricted range of motion
Skin changes, such as thickening or hardening
Frequent infections in the affected area
Unlike lipedema, lymphedema can develop gradually and may worsen over time if not properly managed. Patients may also experience discomfort and psychological impacts due to the visible swelling, which can lead to social withdrawal or anxiety. Early intervention is critical, as it can help manage symptoms and prevent complications such as skin infections or lymphangiosarcoma, a rare but serious complication associated with untreated lymphedema. Regular monitoring and a proactive approach to treatment can significantly enhance the quality of life for those affected by this condition.
Key Differences Between Lipedema and Lymphedema
 Fat Distribution and Symptoms
Fat Distribution and Symptoms
One of the most significant differences between lipedema and lymphedema lies in the distribution of fat and swelling. In lipedema, the swelling is often symmetrical and primarily affects the lower body, while lymphedema can cause asymmetric swelling in any part of the body.
Additionally, lipedema is characterized by a specific type of fat that is resistant to weight loss, whereas lymphedema involves fluid accumulation due to lymphatic dysfunction. Patients with lipedema often report a feeling of heaviness and tenderness in the affected areas, which can lead to discomfort during physical activity.
In contrast, lymphedema may present with a feeling of tightness or fullness, and patients may experience frequent infections in the swollen areas due to compromised lymphatic drainage.
Diagnosis and Assessment
Diagnosing lipedema and lymphedema involves a thorough clinical assessment. Healthcare professionals typically consider the patient's medical history, physical examination, and sometimes imaging studies to differentiate between the two conditions. Key diagnostic criteria include:
In addition to these criteria, healthcare providers may also utilize patient-reported outcomes to gauge the impact of these conditions on daily life. For instance, individuals with lipedema may express frustration regarding their body image and the emotional toll of living with a condition that is often misunderstood.
On the other hand, patients with lymphedema may emphasize the challenges of managing their condition, particularly in relation to mobility and the risk of developing complications such as cellulitis.
Treatment Approaches
Both conditions require different treatment strategies tailored to their unique characteristics. While there is no cure for either condition, management can significantly improve quality of life.
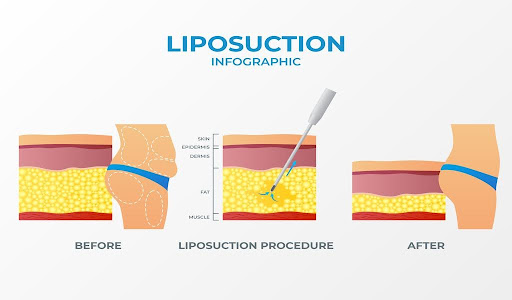
Lipedema: Treatment often focuses on lifestyle changes, such as dietary modifications and exercise. Compression garments may help manage symptoms, and in some cases, surgical options like liposuction can be considered to remove excess fat.
Additionally, support groups and counseling can provide emotional support and education, helping patients navigate the psychological aspects of living with lipedema.
Lymphedema: Management typically includes compression therapy, manual lymphatic drainage, and exercises designed to promote lymphatic flow. In severe cases, surgical interventions may be necessary to restore lymphatic function.
Furthermore, ongoing education about skin care and infection prevention is crucial, as patients must be vigilant in protecting their skin from injuries that could lead to complications.
Understanding the appropriate treatment options is essential for effective management and improving patient outcomes. Both conditions highlight the importance of a multidisciplinary approach, involving specialists such as dietitians, physical therapists, and mental health professionals to address the comprehensive needs of individuals affected by these disorders.
Living with Lipedema and Lymphedema
 Emotional and Psychological Impact
Emotional and Psychological Impact
Both lipedema and lymphedema can have profound emotional and psychological effects on individuals. The visible changes in body shape and the physical limitations caused by these conditions can lead to feelings of self-consciousness, anxiety, and depression. Support groups and counseling can provide valuable resources for coping with these challenges. Many individuals report a sense of isolation, as friends and family may not fully understand the complexities of living with these conditions. This lack of understanding can exacerbate feelings of loneliness and frustration, making it essential for those affected to seek out communities where they can share their experiences and find validation.
Engaging in therapeutic practices such as mindfulness and cognitive-behavioral therapy can also help individuals develop healthier coping mechanisms and improve their overall mental well-being.
Importance of Support Networks
Building a support network is crucial for individuals living with either condition. Connecting with others who understand the challenges can provide emotional support and practical advice. Online forums, local support groups, and professional counseling can be beneficial in fostering a sense of community and shared experience.
Additionally, these networks often serve as a platform for sharing resources, such as recommendations for specialists, treatment options, and lifestyle adjustments that can make daily life more manageable. The power of shared stories can not only inspire hope but also empower individuals to take an active role in their own health journeys. Many support groups even organize events and workshops that focus on education, self-care techniques, and advocacy, further strengthening the bonds among members.
Education and Advocacy
Education plays a pivotal role in managing both lipedema and lymphedema. Patients should be encouraged to learn about their conditions, treatment options, and self-care strategies. Advocacy efforts aimed at raising awareness about these conditions can also help improve access to care and support for those affected. Increased awareness can lead to better diagnostic practices among healthcare providers, ensuring that individuals receive timely and appropriate treatment.
Furthermore, educational initiatives can help dispel myths and misconceptions surrounding these conditions, fostering a more informed public. Workshops, webinars, and informational pamphlets can serve as valuable tools for both patients and their families, equipping them with the knowledge needed to navigate the complexities of living with lipedema and lymphedema effectively. By becoming advocates for their own health, individuals can also inspire others to seek help and support, creating a ripple effect that benefits the broader community.
Let’s Tackle Lipedema/Lymphedema Together with Doctronic!
Understanding the differences between lipedema and lymphedema is essential for effective diagnosis and treatment. While both conditions involve swelling and can significantly impact quality of life, they have distinct characteristics, causes, and management strategies. By raising awareness and promoting education, individuals can better navigate their journeys with these conditions, leading to improved outcomes and enhanced well-being.
Struggling with lipedema or lymphedema? Discover the key differences between lipedema and lymphedema, two often-misunderstood conditions that impact daily life. Learn how to identify symptoms, explore treatment options with Doctronic, and take proactive steps toward better health.



 Understanding Lipedema
Understanding Lipedema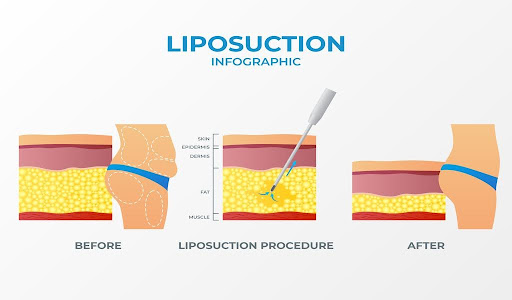 Fat Distribution and Symptoms
Fat Distribution and Symptoms Emotional and Psychological Impact
Emotional and Psychological Impact