Seeing blood in the toilet, on toilet paper, or mixed with a bowel movement can be alarming. While not every case signals a life-threatening condition, the presence of blood in stool is a symptom that warrants attention. This article explains the most common causes, how clinicians evaluate bleeding, when to seek urgent care, and how modern telehealth options, including Doctronic.ai, can help get fast, reliable guidance and follow-up care.
Why Blood in Stool Should Never Be Dismissed
Blood in stool is a clear sign that bleeding is occurring somewhere in the gastrointestinal (GI) tract. The source can be as benign as a small anal fissure or as serious as colorectal cancer. Ignoring it may delay diagnosis of conditions that are easier to treat when caught early.
Even if bleeding seems minor or stops on its own, it still signals that the body experienced some trauma or disease process. Early evaluation can identify treatable causes, prevent complications like anemia or infection, and provide peace of mind.
 How Common Is This Symptom?
How Common Is This Symptom?
Minor rectal bleeding is relatively common over a lifetime: many people experience hemorrhoids or fissures at some point. However, the frequency varies by age and risk factors. Importantly, the probability that bleeding reflects a serious disorder increases with age, family history of colorectal cancer, changes in bowel habits, weight loss, or systemic symptoms like fever or fatigue.
Common Causes of Blood in Stool, from Least to Most Concerning
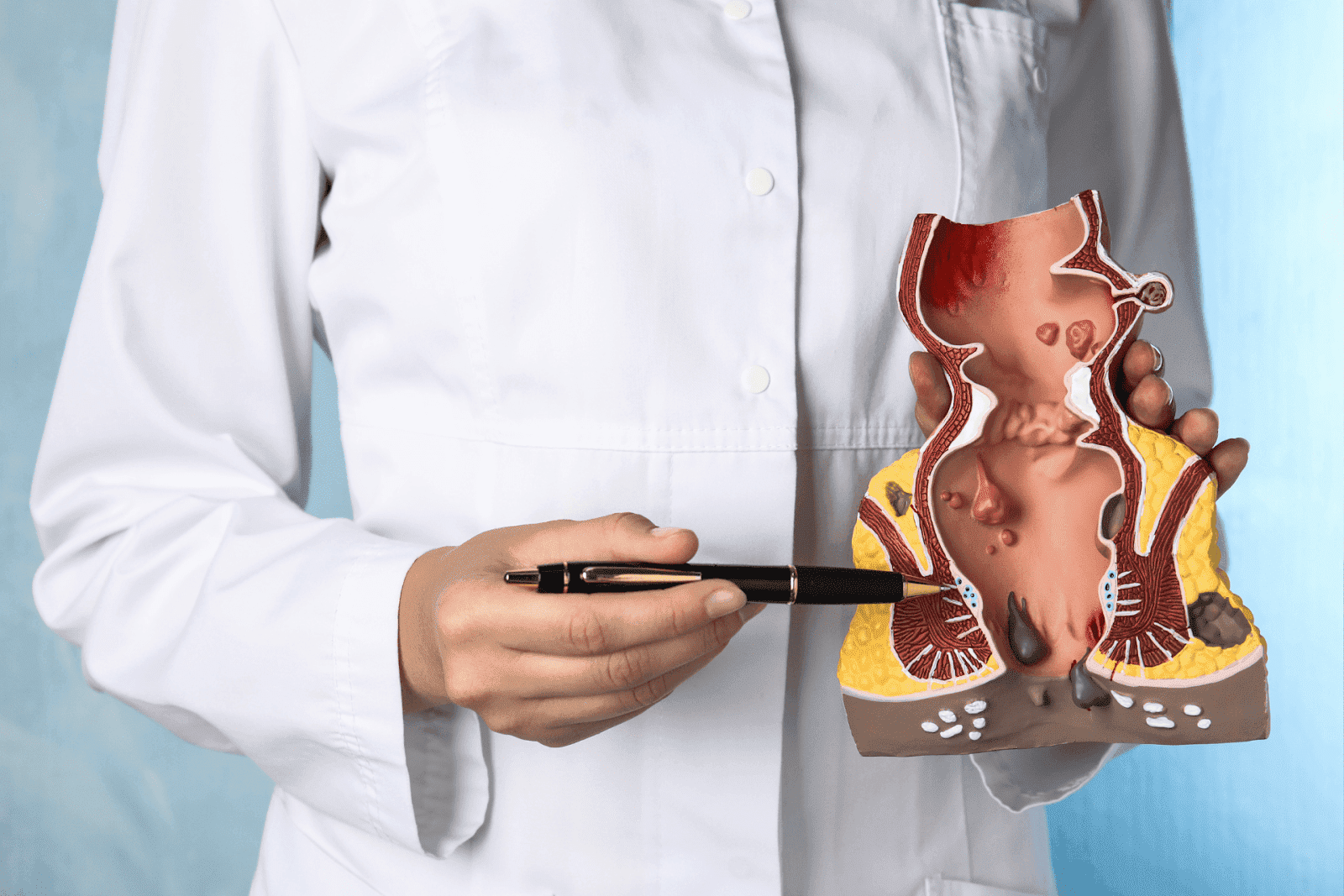
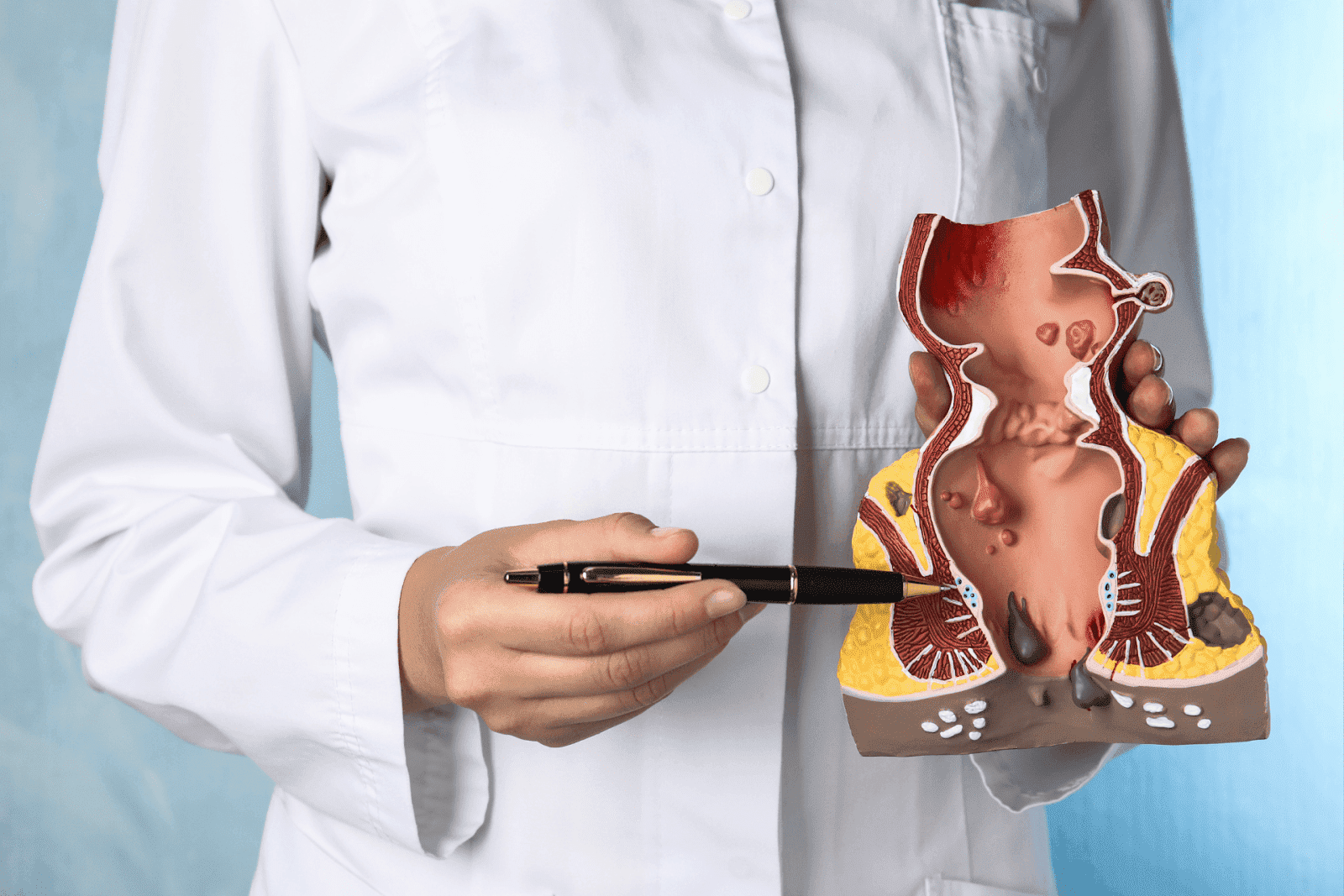
Understanding the range of causes helps prioritize evaluation. Causes fall along a spectrum from benign anorectal conditions to serious disorders in the colon or small intestine.
1. Hemorrhoids
Enlarged veins in the anus and lower rectum are a leading cause of bright red blood on toilet paper or at the end of a bowel movement. Hemorrhoids often cause minimal pain (unless thrombosed) and are common in pregnant people, those with chronic constipation, or anyone who strains frequently.
2. Anal Fissures
Tears in the lining of the anus, often from passing hard stools, cause sharp pain with bowel movements and small amounts of bright red blood. Fissures are usually visible on examination and respond well to conservative measures such as stool softeners, topical treatments, and sitz baths.
3. Diverticulosis and Diverticulitis
Diverticula are small pouches in the colon wall. When they bleed, bleeding may be brisk and cause darker red or maroon stools, often without pain. If a pouch becomes inflamed or infected (diverticulitis), symptoms include localized abdominal pain, fever, and sometimes bleeding.
4. Polyps and Colorectal Cancer
Polyps are benign growths that can bleed intermittently; some types can progress to colorectal cancer over time. Colorectal cancer is a leading cause of cancer death worldwide, but it is highly treatable when detected early. Not every bleeding episode is cancer, but any unexplained rectal bleeding, especially in people over age 45 (or earlier with risk factors), should prompt evaluation.
5. Inflammatory Bowel Disease (Crohn’s Disease and Ulcerative Colitis)
IBD causes chronic inflammation of the digestive tract and commonly produces bloody diarrhea, abdominal pain, and systemic symptoms like fatigue and weight loss. Inflammatory causes often include persistent diarrhea, mucus in the stool, and possible extraintestinal signs such as joint pain.
6. Infections and Ischemic Colitis
Certain bacterial infections (Salmonella, Shigella, Campylobacter, E. coli) and parasitic organisms can cause bloody diarrhea. Ischemic colitis, reduced blood flow to the colon, produces sudden abdominal pain and bloody stools, typically in older adults with vascular disease.
7. Medications and Bleeding Disorders
Anticoagulants (blood thinners), nonsteroidal anti-inflammatory drugs (NSAIDs), and some supplements can increase bleeding risk. Underlying bleeding disorders or thrombocytopenia may also present with GI bleeding. Medication reviews and blood tests are essential parts of the evaluation.
What to Look for When Blood Appears in Stool
Noticing details about the bleeding helps guide clinicians to likely causes. Keep track of the color, accompanying symptoms, and frequency.
Color and Pattern Matter
Bright red blood often means bleeding from the lower GI tract (rectum or sigmoid colon) or from hemorrhoids. Dark red, maroon, or black, tarry stools can indicate bleeding higher in the GI tract. However, stool color may be affected by diet, iron supplements, or bismuth-containing compounds, so the clinical context is important.
Associated Symptoms to Note
Record symptoms such as abdominal pain, fever, changes in bowel habits (constipation or diarrhea), weight loss, lightheadedness, or shortness of breath. Also note how much blood was seen, whether it was on the surface of the stool, mixed in, or clotted, and how often episodes occur.
How Clinicians Evaluate Blood in Stool
Evaluation begins with a medical history and physical exam, followed by targeted tests. Many evaluations can start remotely via telehealth and then proceed to in-person diagnostics if needed.
Initial History and Exam
Clinicians ask about duration and pattern of bleeding, medical history (including medications and family history of colorectal cancer), and accompanying symptoms. A rectal exam can be performed in-person to check for hemorrhoids or fissures; otherwise, a telehealth visit can triage urgency and recommend next steps.
Tests That May Be Ordered
Common tests include fecal occult blood testing or fecal immunochemical testing (FIT) for occult blood, complete blood count (CBC) to check for anemia, stool studies for infection, and cross-sectional imaging such as a CT scan in select cases. Colonoscopy is the gold-standard diagnostic and therapeutic procedure for lower GI bleeding, allowing visualization, biopsy, and polyp removal.
When to Seek Immediate Care
Some scenarios require urgent evaluation in an emergency setting.
Seek Emergency Care If:
There is heavy bleeding or passage of large clots, causing dizziness, fainting, or faintness.
Blood is bright red and continuous, or there are signs of shock (pale skin, rapid heartbeat, confusion).
There is severe abdominal pain, persistent vomiting, high fever, or signs of infection.
There is bleeding, and the person is on anticoagulant therapy or has a known bleeding disorder.
For non-emergent but concerning symptoms (new rectal bleeding, persistent or recurrent bleeding, or blood plus changes in bowel habits), prompt evaluation within days is appropriate.
How Telehealth Can Help: Fast Triage, Expert Guidance, and Follow-Up
Telehealth is an efficient way to start the diagnostic process, especially for non-emergent bleeding. A virtual visit enables quick assessment of risk, guidance on home care, and coordination of testing or in-person referrals when needed.
Doctronic.ai offers both free AI doctor visits and affordable (<$40) video visits with licensed clinicians 24/7 across all 50 states, making it easy to get an initial evaluation without waiting weeks for an appointment. The Doctronic AI synthesizes the latest peer-reviewed medical research to provide evidence-backed guidance instantly, and live telehealth video visits allow for prescription, ordering tests, and arranging urgent referrals if necessary. Learn more or start with a visit to Doctronic.ai.
What a Telehealth Visit Can Accomplish
During a virtual visit, clinicians can review symptoms, examine visible findings via video (when appropriate), advise on whether emergency care is needed, and arrange laboratory tests or a colonoscopy referral. Telehealth also provides convenient follow-up to discuss test results and next steps without additional travel or long waits.
Tests and Treatments Commonly Used
Treatment depends on the cause. Tests confirm the diagnosis and guide appropriate therapy.
Diagnostic Tests Explained
Colonoscopy: The most definitive test for lower GI bleeding. It visualizes the entire colon, allows biopsies, and treats polyps or bleeding lesions. Fecal tests (FIT or stool guaiac) detect occult blood. Stool cultures identify infectious causes. CT angiography or tagged red blood cell scans are used in cases of significant acute bleeding to localize the source.
Treatment Options
Management ranges from conservative measures to procedural interventions. Hemorrhoids and fissures are treated with dietary changes, topical therapies, and stool softeners. Inflammatory bowel disease requires anti-inflammatory and immunosuppressive medications. Infections are treated with targeted antibiotics or antiparasitic agents. Polyps are removed during colonoscopy; cancers require multidisciplinary care, including surgery, chemotherapy, or radiation, depending on stage.
Preparing for a Medical Visit: What Information Helps Clinicians
Being ready with specific information makes visits, whether virtual or in-person, more efficient and effective.
Key Details to Provide
Share when bleeding started, how much and how often it occurs, stool appearance, associated symptoms (pain, fever, weight loss), recent travel or antibiotic use, and a complete medication list including supplements. Mention personal or family history of colorectal cancer, inflammatory bowel disease, or bleeding disorders.
Useful Photos and Notes
For visible bleeding or changes in the perianal area, secure photos can be shared during telehealth visits to assist evaluation. Keep a brief log of bleeding episodes and any dietary changes, as this can reveal patterns related to food or medication triggers.
Prevention and When to Get Screened
Preventive measures and appropriate screening can reduce the risk of severe conditions, such as colorectal cancer.
Screening Guidelines and Risk-Based Timing
Colorectal cancer screening is recommended for average-risk adults starting at age 45 to 50, depending on guidelines and individual risk. People with a family history of colorectal cancer or certain genetic syndromes should begin screening earlier and may need more frequent surveillance. Screening options include colonoscopy, stool-based testing (FIT or FIT-DNA), and CT colonography in specific circumstances.
 Lifestyle Measures That Help
Lifestyle Measures That Help
High-fiber diets, adequate hydration, regular exercise, limiting alcohol, and avoiding smoking reduce colorectal cancer risk and help prevent constipation-related anorectal trauma. Managing chronic conditions, reviewing medications with a clinician, and treating persistent gastrointestinal symptoms promptly are sensible precautions.
Realistic Expectations: Not Every Bleed Is Catastrophic, but None Should Be Ignored
Many causes of rectal bleeding are benign and treatable. Still, because bleeding can be the first sign of a significant disease, early evaluation is important. Timely assessment leads to better outcomes and often less invasive treatment.
Care decisions should balance urgency and prudence: immediate emergency care is required for heavy bleeding or signs of systemic instability, while telehealth can provide rapid, evidence-based triage for non-emergent cases and arrange appropriate testing and follow-up.
Actionable Next Steps if Blood Appears in Your Stool
Follow this simple, practical checklist to get timely care.
Step-By-Step Guidance
Assess severity: If bleeding is heavy, accompanied by fainting, dizziness, rapid heartbeat, or severe abdominal pain, go to the emergency department immediately.
For non-emergent bleeding, use telehealth for rapid triage. Services such as Doctronic.ai offer free AI assessments and affordable clinician video visits 24/7, enabling quick guidance and test ordering from anywhere in the United States. Start at Doctronic.ai to get immediate help and next-step recommendations.
Keep a record: note color, timing, and associated symptoms. Take photos if there are visible external findings. Prepare a medication list and relevant medical history for the clinician.
Follow recommended testing and specialist referrals, such as colonoscopy when indicated, and adhere to scheduled follow-up. Early detection often results in simpler, more effective treatment.
Final Takeaway
Blood in the stool is a significant warning sign. While not every episode means a severe disease, none should be ignored. Prompt evaluation, starting with a careful history and physical and often initiated through telehealth, helps identify the cause quickly and directs appropriate treatment. Modern telehealth tools, like Doctronic.ai, combine rapid, research-backed AI assessments with affordable, licensed clinician video visits available 24/7 to make it easier to act fast and get the right care.
When in doubt, get evaluated. Early answers can prevent complications and provide peace of mind.
Get Fast, Expert Guidance if You Notice Blood in Your Stool
If you’ve spotted blood in your stool and want a quick, evidence-backed next step, Doctronic, the #1 AI Doctor, gives you a free AI visit that delivers modern, peer-reviewed medical guidance in seconds and can help triage whether you need urgent care, testing, or a specialist. When you're ready to move from answers to action, our licensed clinicians are available for affordable video visits (<$40) 24/7 across all 50 states. Over 10 million people have already trusted Doctronic for faster, smarter, and more personal care. Skip the line. Talk to an AI Doctor Now, for free.



 How Common Is This Symptom?
How Common Is This Symptom? Lifestyle Measures That Help
Lifestyle Measures That Help