Ankle pain is one of the most common musculoskeletal complaints, affecting people of all ages and activity levels. Whether the discomfort follows a twist on the soccer field, develops gradually from overuse, or arrives unexpectedly with swelling and stiffness, understanding the likely causes and the right next steps can make a big difference in recovery. This guide walks through common causes, key symptoms to watch for, diagnostic approaches, self-care measures, and when to seek remote or in-person medical attention. For quick, evidence-based guidance and easy access to telehealth options, Doctronic.ai offers free AI doctor visits and affordable video visits with clinicians across all 50 states.
Why an Ankle Symptom Checker is Useful
An ankle symptom checker helps organize what might otherwise feel like a confusing set of signs: pain location, swelling, bruising, instability, difficulty bearing weight, or changes in range of motion. A structured approach narrows down possibilities, helps prioritize urgent issues, and points to appropriate home care or the need for professional evaluation.
Symptom checkers are not a substitute for clinical diagnosis, but when combined with reliable medical sources, they can speed the path to effective treatment. Doctronic.ai is an accessible example of a tool that synthesizes peer-reviewed medical knowledge and provides both free AI-driven assessments and human telehealth follow-up if needed.
 Common Causes of Ankle Pain
Common Causes of Ankle Pain
Ankle pain arises from structures within and around the joint: bones, ligaments, tendons, cartilage, nerves, and surrounding soft tissues. Here are the most frequent culprits.
Sprains (Ligament Injuries)
Sprains are the most common ankle injury, typically occurring when the foot twists inward (inversion) or less commonly outward (eversion). The lateral ligaments, especially the anterior talofibular ligament, are most often affected. Symptoms include immediate pain, swelling, possible bruising, and difficulty bearing weight. Severity ranges from mild stretching to complete rupture.
Fractures (Broken Bones)
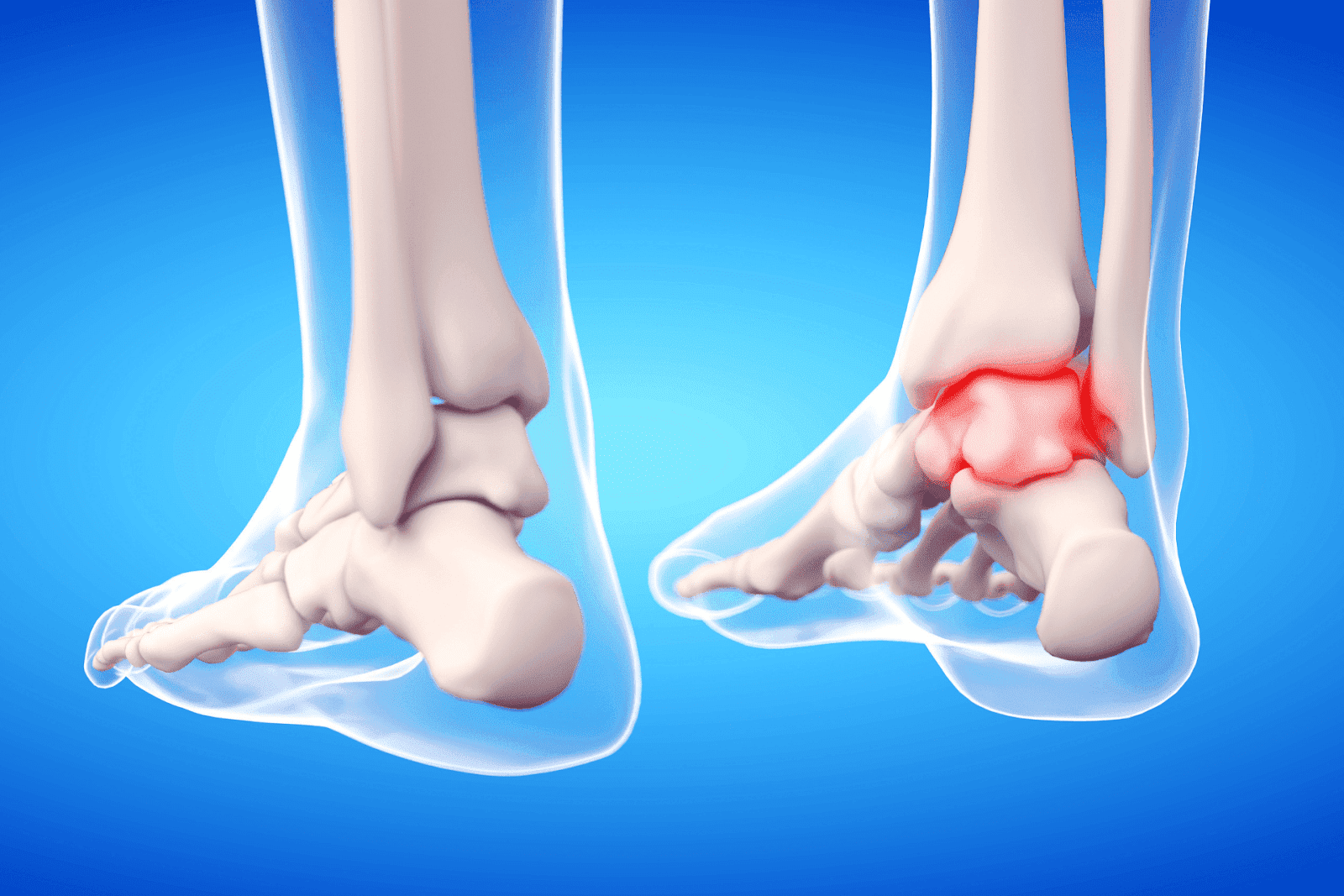
Fractures can involve the tibia, fibula, or talus. They often cause sharp pain, swelling, deformity, and inability to bear weight. High-impact trauma, falls, and sports injuries increase fracture risk. Imaging with X-ray is typically required to confirm the diagnosis.
Tendon Injuries and Tendinopathy
Tendons around the ankle, such as the Achilles tendon or peroneal tendons, can become inflamed (tendinitis), degenerate with overuse (tendinosis), or rupture. Symptoms include localized pain, stiffness (often worse with the first steps in the morning), and weakness. An Achilles rupture may present with a sudden snapping sensation and inability to push off the foot.
Arthritis and Degenerative Disease
Osteoarthritis or post-traumatic arthritis can produce chronic ankle pain, especially with activity. Symptoms develop gradually and include stiffness, swelling after prolonged use, and reduced range of motion. Inflammatory arthritides (for example, rheumatoid arthritis or gout) may cause episodic severe pain with swelling and redness.
Bursitis, Nerve Entrapment, and Referred Pain
Bursitis (inflammation of fluid-filled sacs), nerve entrapment (such as tarsal tunnel syndrome), and pain referred from the knee or hip can all present as ankle pain. These causes are often distinguished by specific patterns: burning or tingling suggests nerve involvement, while localized tenderness over a bursa suggests bursitis.
Key Symptoms to Evaluate and What They Suggest
Breaking down symptoms helps determine whether immediate care is needed and what tests are likely to be helpful.
Pain Timing and Onset
Sudden, severe pain after a specific injury suggests a sprain or a fracture. A gradual onset that worsens with activity points toward tendinopathy or arthritis. Intermittent sharp pain with specific movements may indicate impingement or mechanical problems within the joint.
Swelling, Bruising, and Deformity
Rapid swelling and bruising after injury suggest a ligament tear or fracture. Deformity or an obviously malaligned ankle requires urgent evaluation. Mild swelling that develops slowly is more consistent with overuse injuries or inflammatory arthritis.
Ability to Bear Weight
Being unable to take a few steps after an injury is a red flag for fracture or severe sprain and usually warrants imaging. If the ankle can be used but remains painful with activity, conservative treatment may be appropriate initially.
Instability or "Giving Way"
Chronic instability, such as feeling the ankle will give out, often follows repeated sprains and can indicate ligament laxity. This may benefit from rehabilitation focused on strength and proprioception, bracing, or specialist review.
Simple At-Home Tests to Narrow the Cause
These quick checks help determine whether immediate medical attention or imaging is likely needed.
Observe and Compare
Compare the injured ankle with the opposite side. Look for asymmetry in swelling, color changes, or deformity. Subtle differences can be important clues, and photographs can be useful to track progression.
Palpation
Gently press along the ankle bones and ligaments. Localized bone tenderness, especially over the malleoli (the bony bumps on each side of the ankle), raises concern for fracture. Tenderness over ligaments or tendons suggests sprain or tendinopathy.
Weight-Bearing and Range of Motion
Attempting to stand and walk a few steps can indicate severity: inability to bear weight or marked instability suggests urgent evaluation. Testing ankle dorsiflexion, plantarflexion, inversion, and eversion can help localize the problem. Limited motion with pain often points to joint or soft tissue injury.
When to Seek Immediate Medical Care
Recognizing urgent signs can prevent complications and improve outcomes. Seek immediate in-person medical attention or urgent imaging when any of the following are present after ankle injury:
- Inability to bear weight or walk more than a few steps on the injured ankle.
- Significant deformity or bone protrusion.
- Severe unrelenting pain, rapid swelling, or numbness/tingling.
- Wounds with exposed bone or deep puncture near the joint.
How Clinicians Diagnose Ankle Problems
A healthcare provider combines history, physical exam, and selective imaging or tests to make a definitive diagnosis.
Clinical Exam
Examination focuses on point tenderness, ligament tests, range of motion, gait analysis, and neurovascular status. Special maneuvers help identify instability, tendon dysfunction, or nerve irritation.
Imaging
X-rays are the first-line test to evaluate for fractures. Ultrasound can assess tendons and soft tissue injuries at the point of care. MRI provides detailed views of ligaments, cartilage, and bone edema when symptoms persist or complex injuries are suspected.
Lab Tests
When inflammatory or infectious causes are suspected, red, hot, swollen ankle with systemic symptoms, blood tests and possibly joint aspiration may be pursued to identify gout, septic arthritis, or autoimmune conditions.
Evidence-Based Treatment Options
Treatment depends on the diagnosis and severity, but many ankle problems respond well to conservative care when appropriate.
RICE and Early Care
For acute sprains and minor injuries, the initial approach often includes Rest, Ice, Compression, and Elevation (RICE). Limiting weight-bearing and using crutches temporarily can reduce pain and swelling in the first 48–72 hours.
Pain Control and Anti-Inflammatory Strategies
Over-the-counter analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) help manage pain and reduce inflammation. Topical NSAIDs can be an alternative for localized pain. Follow dosing recommendations and consult a clinician for chronic use.
Immobilization and Bracing
Mild sprains may benefit from an ankle brace, while more severe sprains or certain fractures require a short period in a cast or walking boot. Bracing can provide stability and allow ligaments to heal appropriately while avoiding stiffness associated with prolonged immobilization.
Rehabilitation and Physical Therapy
Rehabilitation emphasizes range-of-motion exercises, progressive strengthening, and proprioception (balance) training to restore function and prevent recurrence. Physical therapy is particularly important for recurrent sprains and after immobilization periods.
Surgical Options
Surgery may be necessary for unstable fractures, complete tendon ruptures, or chronic instability refractory to rehabilitation. Surgical techniques and recovery timelines vary by condition and patient factors.
Prevention and Long-Term Ankle Health
Lowering the risk of future ankle injuries involves strength, flexibility, footwear choices, and modifying activities when needed.
Strength and Balance Training
Regular exercises focusing on the calf muscles, peroneals, and intrinsic foot muscles help stabilize the ankle. Single-leg balance drills and wobble-board exercises can be particularly effective at reducing recurrent sprains.
Proper Footwear and Orthotics
Shoes with good ankle support and appropriate soles for the activity reduce awkward twists. For structural foot problems, custom or over-the-counter orthotics may redistribute forces and improve alignment.
Gradual Training Progressions
Avoid abrupt increases in activity, training volume, or intensity. Ramping up gradually and incorporating cross-training reduces overuse injuries and tendon strain.
When Telehealth is a Good Option
Many ankle problems can be triaged effectively via telehealth, especially when images of swelling or bruising are available and the patient can describe the mechanism of injury clearly. Telehealth can provide rapid guidance on whether urgent in-person care or imaging is needed, and it can help with follow-up care and rehabilitation planning.
Doctronic.ai offers free AI-driven symptom checks and inexpensive ($<40) video visits with licensed clinicians 24/7 in all 50 states, which is useful for initial assessment, medication guidance, follow-up of uncomplicated sprains, and determining the need for urgent imaging. Visit Doctronic.ai for a quick, evidence-based evaluation and to schedule affordable telehealth visits.
How to Use an Ankle Symptom Checker Effectively
To get the most from a symptom checker, gather the following information before starting: when the pain began, the mechanism of injury (if any), exact pain location, severity, ability to bear weight, presence of swelling or bruising, and any numbness or systemic symptoms. Including photos or short videos of the ankle while walking can be very helpful for remote clinicians.
Symptom checkers that draw on peer-reviewed medical literature and synthesize guidance quickly, like the AI assessments available through Doctronic.ai, help prioritize next steps and suggest evidence-based self-care. If the symptom checker recommends urgent care or imaging, follow that recommendation promptly.
Red Flags and Atypical Presentations
Not all ankle pain is mechanical. A few signs suggest a more serious or systemic issue:
- High fever, chills, or feeling generally unwell with a hot, red, swollen ankle (possible septic arthritis).
- Sudden severe pain with a known history of gout or elevated uric acid (gout flare).
- Progressive numbness or loss of pulses in the foot (circulatory compromise).
Any of these findings warrants immediate medical attention.
Follow-Up Care and Rebuilding Activity
Recovery timelines vary widely: mild ankle sprains often improve in 1–3 weeks, moderate sprains in 4–8 weeks, and severe injuries or fractures may take months. Return to sport or high-impact activities should be gradual and guided by pain-free strength, range of motion, and performance on sport-specific drills.
Rehabilitation should progress from mobility work to strengthening and then to agility and plyometric exercises as tolerated. Proper guidance from a physical therapist or sports medicine clinician can optimize recovery and reduce recurrence risk.
Practical Checklist: What to do After an Ankle Injury
Stop the activity and assess safety. If severe pain or deformity exists, seek emergency care.
Apply RICE measures in the first 48–72 hours: rest, ice, compression, elevation.
Avoid weight-bearing if unable to take a few steps without significant pain; use crutches or a cane as needed.
Consider over-the-counter pain relief in line with medical guidance.
Use a symptom checker or telehealth service for an early evaluation. Doctronic.ai provides fast AI assessments and affordable video visits with licensed clinicians nationwide.
If symptoms do not improve or worsen over several days, arrange an in-person follow-up and consider imaging.
 When to Expect Improvement and When to Seek Further Care
When to Expect Improvement and When to Seek Further Care
Improvement within the first week is common for mild injuries. If pain, swelling, or instability persists beyond two weeks despite conservative care, or if function is markedly limited, a clinician should reassess to rule out missed fractures, tendon injuries, or the need for more intensive rehabilitation. Persistent or recurrent symptoms may require imaging or referral to orthopedics or sports medicine.
Understand Ankle Pain and Take Action
An organized approach to ankle pain, such as assessing the mechanism, key symptoms, and red flags, helps determine whether self-care, telehealth evaluation, or urgent in-person care is appropriate. Doctronic.ai can provide rapid, evidence-based assessments and convenient follow-ups, including low-cost video visits with licensed clinicians available 24/7 across all 50 states. For many patients, a timely AI-assisted triage followed by appropriate imaging or therapy prevents prolonged disability and speeds return to full activity.
For a quick, reputable symptom check and to connect with clinicians remotely, visit Doctronic.ai and start with a free AI doctor visit or schedule an inexpensive telehealth appointment under $40.
Get Fast, Expert Guidance for Your Ankle Pain
If you’re unsure whether your ankle needs urgent care, start with Doctronic, the #1 AI Doctor. Our AI provides an evidence-based assessment in seconds, remembers your history, and can guide home care or recommend urgent imaging when needed; you can then book an inexpensive (<$40) 24/7 video visit with a licensed clinician in any state. Skip the line. Talk to an AI Doctor Now, for free.



 Common Causes of Ankle Pain
Common Causes of Ankle Pain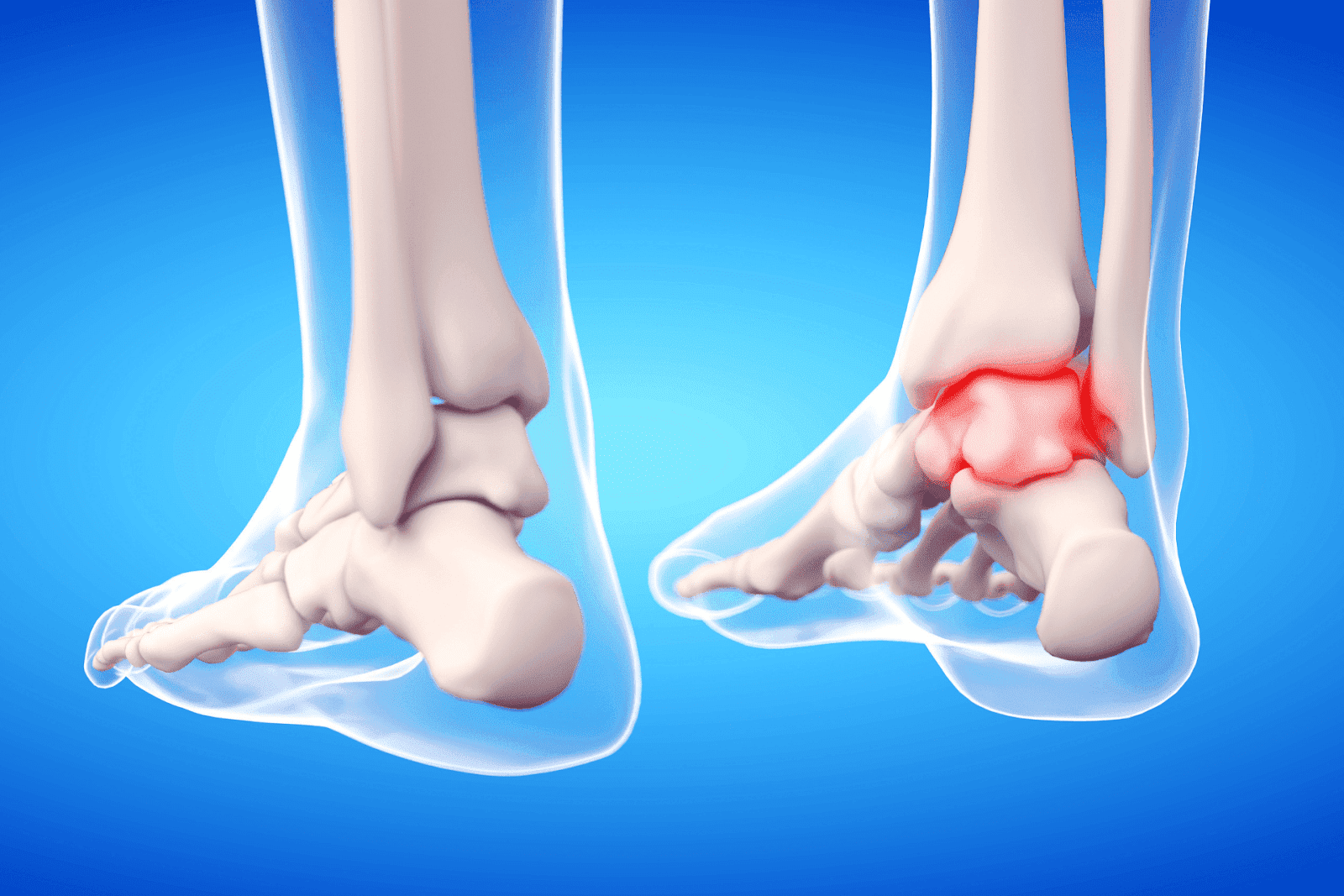 When to Expect Improvement and When to Seek Further Care
When to Expect Improvement and When to Seek Further Care