Joint pain is one of the most common complaints in medical care, affecting millions of adults and many children. Arthritis, an umbrella term for conditions that cause inflammation or degeneration of joints, can interfere with daily life, sleep, work, and physical activity. Recognizing the early signs, understanding the types, and knowing when to seek help are critical steps toward preserving mobility and quality of life.
What “Arthritis” Really Means
Arthritis is not a single disease but a group of conditions characterized by joint pain, stiffness, swelling, and reduced range of motion. Two broad categories account for most cases: inflammatory arthritis (such as rheumatoid arthritis) and degenerative arthritis (osteoarthritis). Other forms include gout, psoriatic arthritis, lupus-related arthritis, and juvenile idiopathic arthritis.
Symptoms arise from different mechanisms: autoimmune inflammation damaging the joint lining and cartilage, crystal deposition causing intense pain and swelling, or wear-and-tear changes that erode cartilage over time. Regardless of the cause, the end result is joint dysfunction and often a reduced ability to do normal activities.
 Common Symptoms to Watch For
Common Symptoms to Watch For
Arthritis symptoms range from mild and intermittent to severe and persistent. Early recognition helps with timely diagnosis and treatment.
Persistent Joint Pain
Pain that lasts weeks to months or worsens with activity is a hallmark symptom. Osteoarthritis pain often increases with use (for example, climbing stairs or standing after sitting), while inflammatory arthritis can cause pain at rest and during the night.
Stiffness, Especially In The Morning
Morning stiffness that lasts longer than 30 minutes tends to suggest inflammatory arthritis like rheumatoid arthritis. Short-lived stiffness after inactivity (lasting less than 30 minutes) is more typical of osteoarthritis.
Swelling and Warmth
Inflamed joints may look swollen, feel warm to the touch, and appear red. Swelling that comes and goes, or affects multiple joints symmetrically (for example, both wrists or both knees), often points toward an inflammatory process.
Reduced Range of Motion and Functional Limitations
Difficulty gripping objects, climbing stairs, or rising from a chair can indicate progressive joint damage. Joint deformities in advanced disease, such as ulnar deviation of the fingers in rheumatoid arthritis, signal longstanding inflammation or degeneration.
Systemic Symptoms
Conditions like rheumatoid arthritis or lupus may cause systemic features, including fatigue, low-grade fevers, weight loss, or involvement of other organs (skin, lungs, eyes). These extra-articular signs require prompt medical evaluation.
How Different Types of Arthritis Present
Understanding how specific forms of arthritis tend to behave helps narrow down the cause and guide testing and treatment choices.
Osteoarthritis (OA)
Osteoarthritis is the most common form and is typically age-related. It results from degeneration of cartilage and adaptive changes in bone. Symptoms usually develop gradually and often affect weight-bearing joints such as knees and hips, as well as hands and the spine.
OA pain usually worsens with activity and improves with rest. Morning stiffness is brief. Imaging (X-rays) may show joint space narrowing, bone spurs, and changes to joint surfaces.
Rheumatoid Arthritis (RA)
Rheumatoid arthritis is an autoimmune disorder that commonly affects smaller joints symmetrically, wrists, finger joints, and toes, and often leads to prolonged morning stiffness and persistent swelling. Without treatment, RA can cause joint erosions and deformity, and may involve the heart, lungs, or eyes.
Gout
Gout typically causes sudden, intensely painful attacks, often starting in the big toe. Attacks are associated with redness, swelling, and extreme tenderness. The underlying problem is crystal deposition (monosodium urate) in and around joints. Blood tests and joint aspiration help confirm the diagnosis.
Psoriatic Arthritis and Other Spondyloarthropathies
Psoriatic arthritis can affect the joints asymmetrically and often involves the skin, psoriasis, along with nail changes and dactylitis (“sausage” digits). Back pain from inflammatory spondyloarthropathy often improves with gentle activity and may be associated with morning stiffness.
Juvenile Arthritis
Arthritis is not only an adult disease. Children can develop juvenile idiopathic arthritis, which may present with a persistent limp, swollen joint, or prolonged fever of unknown cause. Early diagnosis is important to prevent growth problems and reduce long-term disability.
When to Seek Medical Care
Not every ache warrants urgent evaluation, but certain features require prompt attention. See a healthcare provider if joint pain is severe, persistent, or accompanied by fever, significant swelling, rapid worsening, or difficulty using the joint.
Immediate medical attention is needed if the joint is hot, extremely tender, or associated with systemic symptoms like high fever. These signs could indicate septic arthritis, which is an infection inside the joint that can rapidly destroy cartilage and spread to the bloodstream.
Mild, intermittent pain without swelling can be monitored short-term, but repeated or progressive symptoms warrant evaluation because early treatment of many arthritis types improves long-term outcomes.
How Arthritis Is Diagnosed
Diagnosis combines history, physical exam, laboratory tests, and imaging. A careful history examines symptom onset, pattern, associated symptoms, family history, and risk factors such as previous joint injury or repetitive stress.
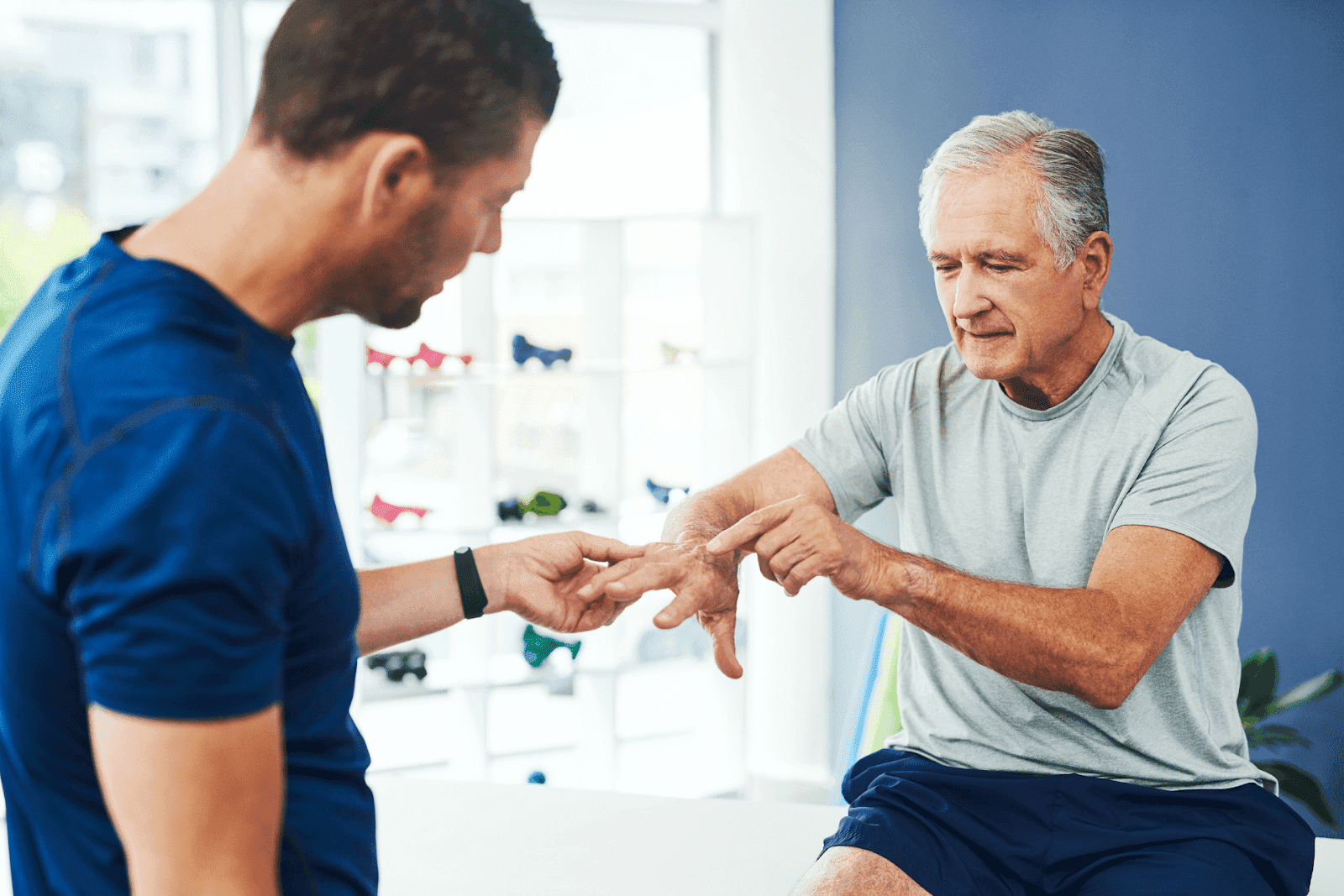
Physical Exam
Joint examination looks for warmth, swelling, tenderness, crepitus, and deformity. Symmetry of involvement and number of joints affected provide essential clues. A full musculoskeletal assessment considers gait, range of motion, muscle strength, and nearby tendons or bursae.
Laboratory Tests
Blood tests can identify inflammatory markers (CRP, ESR), autoantibodies (rheumatoid factor, anti-CCP), and uric acid levels when gout is suspected. Joint aspiration, removing fluid with a needle, is the gold standard to diagnose septic arthritis and crystal-induced arthritis.
Imaging
Plain X-rays detect osteoarthritic changes and advanced erosions. Ultrasound and MRI provide more sensitive detection of early inflammation, soft-tissue changes, and cartilage or bone marrow lesions. Imaging choice depends on the suspected diagnosis and clinical questions.
Treatment Options: Goals and Common Strategies
Arthritis treatment aims to reduce pain, preserve joint function, prevent progression, and improve quality of life. Approaches combine non-drug measures, medications, procedures, and sometimes surgery.
Lifestyle and Nonpharmacologic Care
Weight loss reduces stress on weight-bearing joints and is one of the most evidence-backed interventions for osteoarthritis. Low-impact exercise (walking, swimming, cycling) strengthens muscles and improves flexibility. Physical therapy and occupational therapy teach joint-protecting strategies and adaptive devices.
Heat and cold therapies, assistive devices (such as braces and canes), and ergonomic adjustments at work can also reduce symptoms and enhance daily functioning.
Medications
Acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used for pain control. Topical NSAIDs are effective for localized osteoarthritis pain of the knees and hands. For inflammatory arthritis, disease-modifying antirheumatic drugs (DMARDs), including methotrexate and biologic agents, are used to suppress immune-driven damage.
Gout flares respond to colchicine, NSAIDs, or corticosteroids, while urate-lowering therapy prevents future attacks. Corticosteroid injections into joints can provide temporary relief when inflammation is localized.
Procedures and Surgery
Viscosupplementation, joint aspiration, and corticosteroid injections are common office-based interventions. Joint replacement surgery (such as hip or knee arthroplasty) is highly effective for end-stage osteoarthritis that does not respond to conservative measures.
Managing Symptoms Day-To-Day
Small daily choices often add up to meaningful benefits for joint health. Practical strategies can reduce flare frequency and preserve independence.
Activity Modification and Exercise
Choose low-impact activities and break repetitive tasks into shorter sessions. Strength training supports joints by improving muscle support, while flexibility exercises maintain the range of motion. A physical therapist can create a personalized program.
Pacing and Joint Protection
Pacing activities and using larger joints or tools to distribute load prevent overuse. Ergonomic kitchen tools, jar openers, and adaptive keyboards make routine tasks easier and less painful.
Sleep and Mental Health
Chronic pain commonly disrupts sleep and contributes to anxiety or depression. Cognitive behavioral strategies, sleep hygiene, and treatment for mood disorders, when present, enhance overall symptom management.
Quick, Accessible Care With Doctronic
Telehealth makes it easier for people with joint pain to connect with care quickly, ask questions about symptoms, and decide on the next steps. Virtual visits can be used to assess symptoms, review imaging and lab results, adjust medications, and provide ongoing management without travel or long waits.
Doctronic.ai offers two complementary options: a free AI-driven visit that provides an immediate, evidence-based synthesis of possible causes and next steps, and inexpensive telehealth video visits with licensed clinicians available 24/7 in all 50 states for less than $40. With more than 10 million users and rapid growth, Doctronic positions itself as the #1 AI Doctor, synthesizing peer-reviewed medical knowledge to produce tailored recommendations and remember each patient's history over time. For quick guidance on new or worsening joint symptoms, start at Doctronic.ai and follow up with a clinician when needed.
When to See a Specialist
Primary care clinicians manage many forms of arthritis, but referral to a rheumatologist or orthopedic surgeon can be appropriate in several situations. A rheumatologist is essential when autoimmune or inflammatory arthritis is suspected, when diagnosis is uncertain, or when advanced immunomodulatory treatments are being considered.
An orthopedic surgeon is consulted for structural problems amenable to surgery, such as severe osteoarthritis requiring joint replacement. Timely consultation helps prevent irreversible joint damage and optimizes outcomes.
Preventive Measures and Risk Reduction
Not all arthritis is preventable, but certain steps reduce risk and slow progression. Maintain a healthy weight to decrease joint load, practice good posture and body mechanics to protect joints, and remain physically active to preserve muscle support and flexibility.
For people with repetitive occupational joint stress, ergonomic interventions and periodic breaks can lower long-term injury risk. For gout, dietary changes and medication adherence prevent recurrent flares and joint damage.
Common Myths and Misconceptions
Myths about arthritis can delay care or lead to ineffective treatments. Clearing up common misconceptions helps people make informed choices.
“Arthritis Is Just a Normal Part of Aging”
Aging increases risk for some joint changes, but arthritis is not an inevitable sentence. Many cases benefit from early intervention, lifestyle changes, and targeted treatments.
“Exercise Makes Arthritis Worse”
While acute overuse can exacerbate pain, appropriately tailored exercise generally improves pain, function, and mood. Supervised programs minimize injury risk.
“There’s Nothing That Can Be Done”
Modern treatments, from medications to physical therapy and surgery, often reduce pain and improve function. Autoimmune arthritis is now managed more effectively than in previous decades thanks to early use of disease-modifying therapies.
Practical Steps If Joints Feel Off Today
If a joint becomes sore or swollen, a few immediate actions can be helpful: rest the joint, apply ice if swelling and recent injury are present, and use over-the-counter pain relievers if appropriate. Keep the joint elevated and avoid activities that sharply increase pain.
When symptoms persist beyond a week, worsen, or are accompanied by fever, seek medical evaluation. For fast, evidence-based assessment and guidance, try Doctronic.ai’s free AI visit to get immediate insight, and schedule an inexpensive telehealth video visit with a clinician if a personal evaluation is necessary.
New Treatments and Research Directions
Advances in understanding immune pathways, cartilage biology, and pain modulation have led to new treatments and ongoing research. Biologic drugs and targeted small molecules have revolutionized care for many inflammatory arthritides, while regenerative approaches such as stem cell therapies and tissue engineering are under investigation for cartilage repair.
Telehealth and AI are changing the way care is delivered: more precise, timely triage, and personalized treatment plans based on the latest peer-reviewed evidence. Services that combine AI-driven recommendations with access to clinicians provide a promising avenue for more convenient, consistent care.
 Take Symptoms Seriously and Act Early
Take Symptoms Seriously and Act Early
Joint pain should not be ignored, especially when it limits daily life, is accompanied by swelling, or persists. Understanding symptom patterns, seeking timely evaluation, and combining lifestyle measures with appropriate medical treatment can greatly reduce the burden of arthritis.
For quick guidance and easy access to clinicians, consider starting with Doctronic.ai’s free AI visit for an immediate, evidence-based assessment, and follow up with an inexpensive telehealth video visit if personalized care is needed. Early attention helps protect mobility and maintain an active life.
Get Quick, Personalized Guidance For Joint Pain
If your joints are bothering you now, Doctronic, the #1 AI Doctor headquartered in NYC and trusted by over 10 million users, can help you act fast. Our free AI visit gives an immediate, evidence-based assessment drawn from the latest peer‑reviewed medicine and remembers your history over time; when you need a live clinician, inexpensive telehealth video visits are available 24/7 in all 50 states for under $40. Backed by top-tier seed funding and built to make modern care faster, smarter, and more personal, Doctronic lets you skip waitlists and get clear next steps for diagnosis and treatment. Skip the line. Talk to an AI Doctor Now, for free.



 Common Symptoms to Watch For
Common Symptoms to Watch For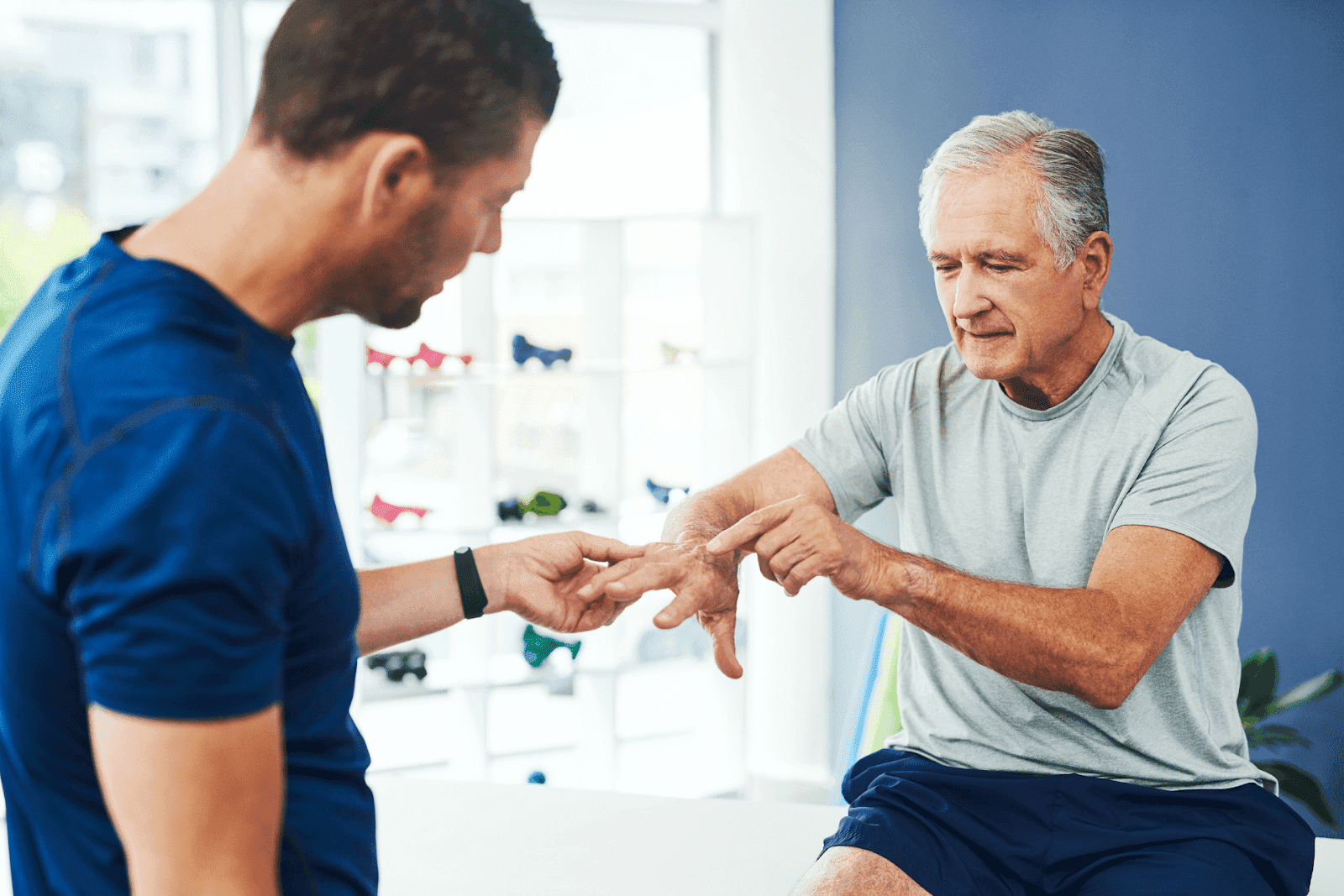 Take Symptoms Seriously and Act Early
Take Symptoms Seriously and Act Early